Tuesday Poster Session
Category: IBD
P4390 - Clinical and Microbiome Effects of Antibiotic Treatment for E. coli Subtypes in IBD Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Defne Ercelen, BSc
NYU Langone Health Inflammatory Bowel Disease Center
New York, NY
Presenting Author(s)
Defne Ercelen, BSc1, Jing Yu Carolina Cen Feng, 1, Benjamin Pundyk, 2, Joseph N. Pucella, PhD2, Jordan Axelrad, MD, MPH2
1NYU Langone Health Inflammatory Bowel Disease Center, New York, NY; 2NYU Grossman School of Medicine, New York, NY
Introduction: The presence of Escherichia coli subtypes in the context of inflammatory bowel disease (IBD) flares is debated. Given the inconsistent attribution of E. coli subtypes as clinically significant infections versus bystanders of intestinal inflammation, there is inconsistent utilization of antimicrobials. Here, we aimed to track the microbiome and clinical outcomes of patients with IBD flare complicated by an E. coli subtype to assess the impact of those treated with an antibiotic.
Methods: This was a prospective, observational study of symptomatic patients with IBD who tested positive for Enteropathogenic E. coli
(EPEC) or Enteroaggregative E. coli (EAEC) by the BioFire FilmArray Gastrointestinal Panel. Patient demographics, IBD characteristics, laboratory values, and utilization and type of antimicrobial was recorded from electronic health records. Stool samples were collected at three time points: baseline at PCR testing, week 2, and month 2, which were analyzed via 16s sequencing. Subsequent IBD outcomes were observed over one year. Qiime2 software was used to analyze the microbiome samples. Fisher’s exact test was used to compare frequencies and means between the two groups.
Results: We identified 28 symptomatic patients with IBD (n= 10 Crohn’s disease, n= 18 ulcerative colitis) and the presence of EPEC (n= 16) or EAEC (n= 12). Of all patients, (17.8%) received antibiotic treatment and (82.2 %) did not (Table). No statistically significant differences were observed between the two groups regarding demographics, IBD therapies, laboratory values, and alpha diversities. Although there was a declining trend in the alpha diversity of the antibiotic treatment group at 2 weeks, the difference was not statistically significant. Alpha diversities of the two groups equalized by the month 2 assessment. Only (n= 2) 40% of the antibiotic treatment group cleared their E. coli subtype over time. A principal coordinate analysis using Bray-Curtis distances showed that the antibiotic treatment group did not cluster separately from the no antibiotic treatment group (Figure). There were no short or long term differences in IBD outcomes over one year between groups.
Discussion: There was no significant clinical impact of antibiotic utilization for the presence of an E.coli subtype complicating IBD flare. This is further supported by molecular evidence, as we could not detect a difference in microbiome signatures between the two groups over time. Our data require further confirmation with a larger cohort.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Defne Ercelen, BSc1, Jing Yu Carolina Cen Feng, 1, Benjamin Pundyk, 2, Joseph N. Pucella, PhD2, Jordan Axelrad, MD, MPH2. P4390 - Clinical and Microbiome Effects of Antibiotic Treatment for <i>E. coli</i> Subtypes in IBD Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health Inflammatory Bowel Disease Center, New York, NY; 2NYU Grossman School of Medicine, New York, NY
Introduction: The presence of Escherichia coli subtypes in the context of inflammatory bowel disease (IBD) flares is debated. Given the inconsistent attribution of E. coli subtypes as clinically significant infections versus bystanders of intestinal inflammation, there is inconsistent utilization of antimicrobials. Here, we aimed to track the microbiome and clinical outcomes of patients with IBD flare complicated by an E. coli subtype to assess the impact of those treated with an antibiotic.
Methods: This was a prospective, observational study of symptomatic patients with IBD who tested positive for Enteropathogenic E. coli
(EPEC) or Enteroaggregative E. coli (EAEC) by the BioFire FilmArray Gastrointestinal Panel. Patient demographics, IBD characteristics, laboratory values, and utilization and type of antimicrobial was recorded from electronic health records. Stool samples were collected at three time points: baseline at PCR testing, week 2, and month 2, which were analyzed via 16s sequencing. Subsequent IBD outcomes were observed over one year. Qiime2 software was used to analyze the microbiome samples. Fisher’s exact test was used to compare frequencies and means between the two groups.
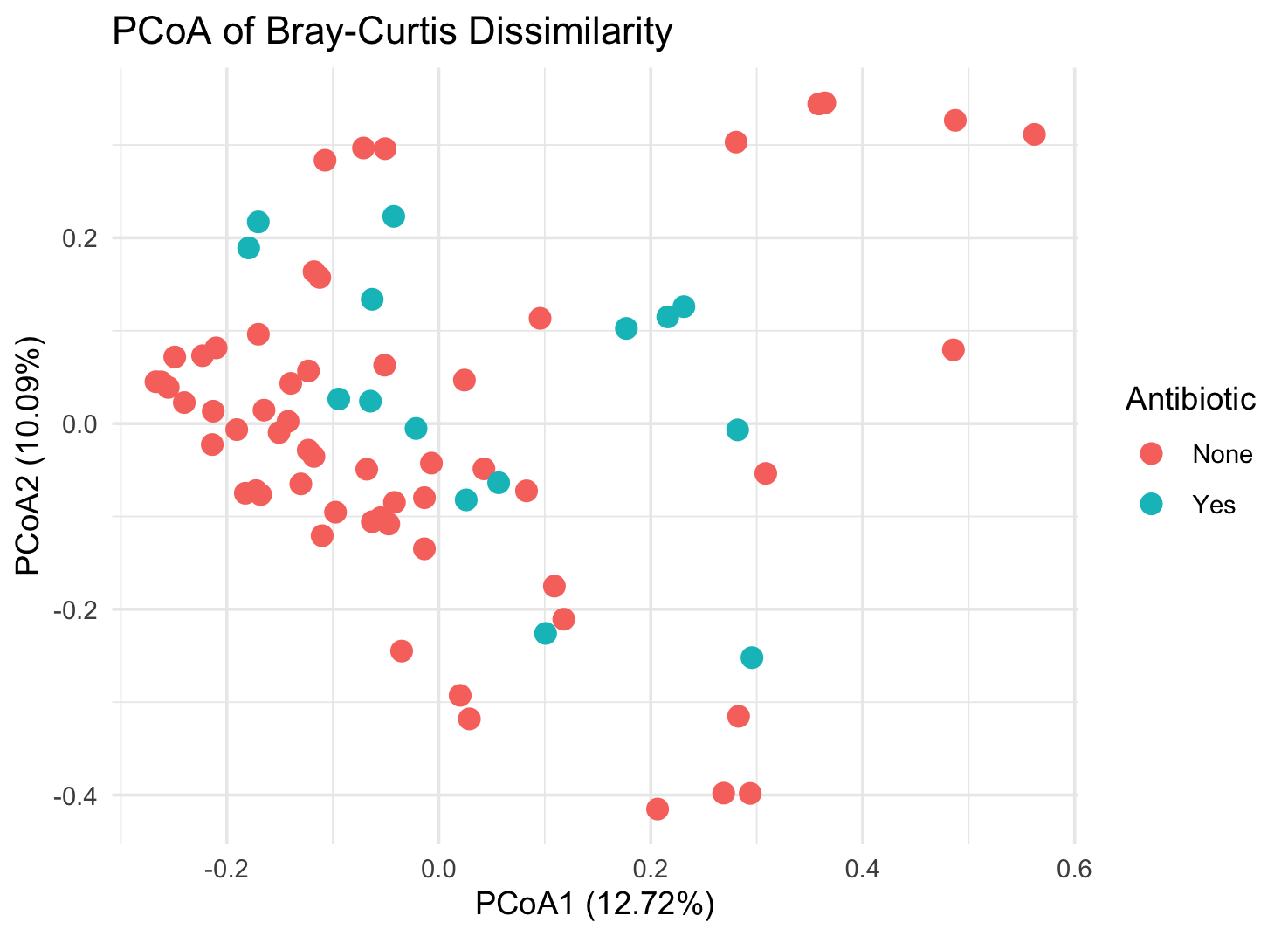
Results: We identified 28 symptomatic patients with IBD (n= 10 Crohn’s disease, n= 18 ulcerative colitis) and the presence of EPEC (n= 16) or EAEC (n= 12). Of all patients, (17.8%) received antibiotic treatment and (82.2 %) did not (Table). No statistically significant differences were observed between the two groups regarding demographics, IBD therapies, laboratory values, and alpha diversities. Although there was a declining trend in the alpha diversity of the antibiotic treatment group at 2 weeks, the difference was not statistically significant. Alpha diversities of the two groups equalized by the month 2 assessment. Only (n= 2) 40% of the antibiotic treatment group cleared their E. coli subtype over time. A principal coordinate analysis using Bray-Curtis distances showed that the antibiotic treatment group did not cluster separately from the no antibiotic treatment group (Figure). There were no short or long term differences in IBD outcomes over one year between groups.
Discussion: There was no significant clinical impact of antibiotic utilization for the presence of an E.coli subtype complicating IBD flare. This is further supported by molecular evidence, as we could not detect a difference in microbiome signatures between the two groups over time. Our data require further confirmation with a larger cohort.
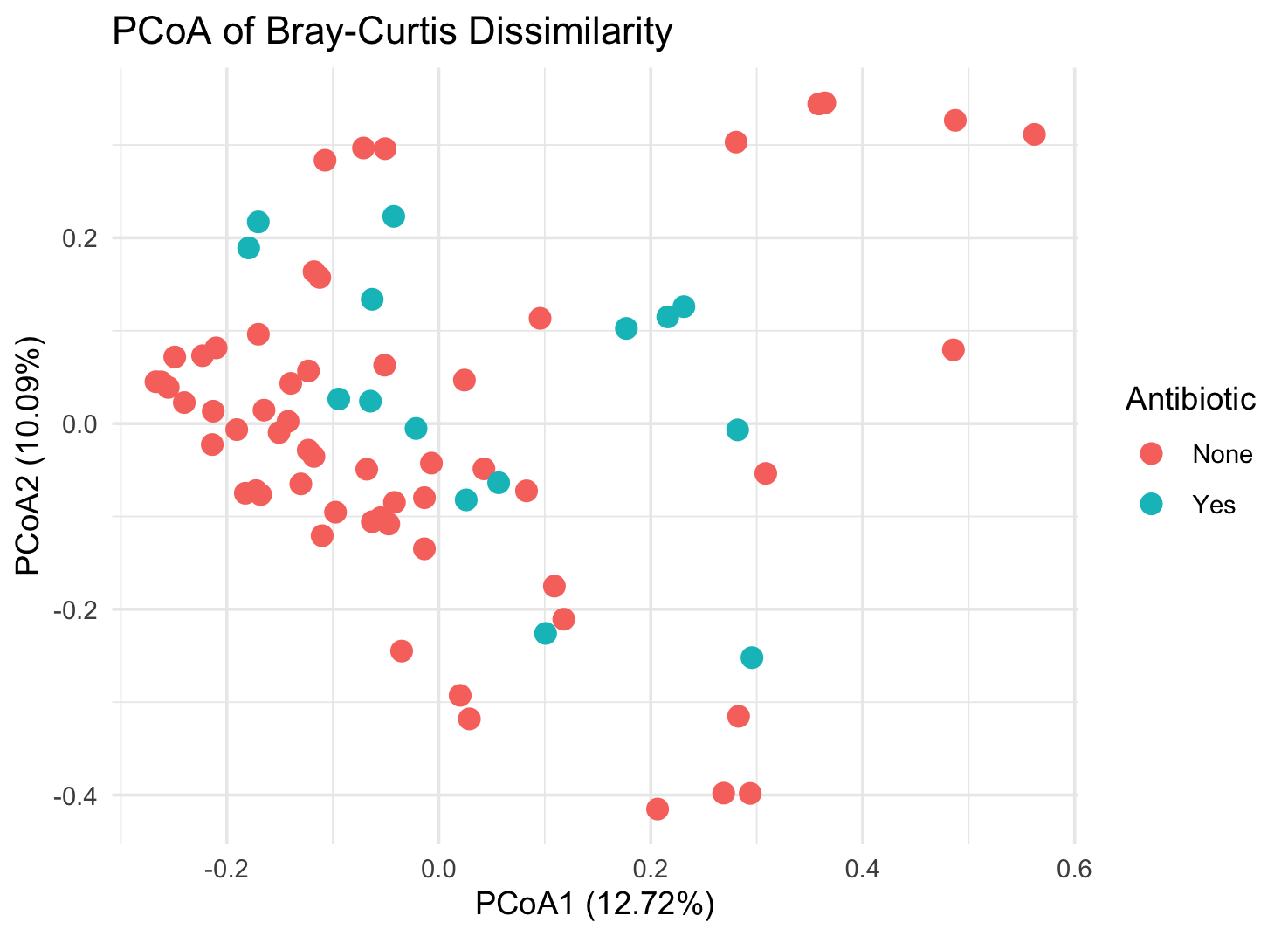
Figure: Figure: Principal coordinate analysis of all samples using Bray-Curtis distances
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Defne Ercelen indicated no relevant financial relationships.
Jing Yu Carolina Cen Feng indicated no relevant financial relationships.
Benjamin Pundyk indicated no relevant financial relationships.
Joseph Pucella indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Defne Ercelen, BSc1, Jing Yu Carolina Cen Feng, 1, Benjamin Pundyk, 2, Joseph N. Pucella, PhD2, Jordan Axelrad, MD, MPH2. P4390 - Clinical and Microbiome Effects of Antibiotic Treatment for <i>E. coli</i> Subtypes in IBD Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
