Tuesday Poster Session
Category: IBD
P4393 - Chromoendoscopy-Guided Endomicroscopy for Dysplasia Surveillance in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Gianarakis, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Michael Gianarakis, MD1, Hasan S. Raza, MD2, Omar T. Ahmed, MD1, Elie Ghoulam, MD3, Sandra Naffouj, MD4, Itishree Trivedi, MD, MS2
1University of Illinois at Chicago, Chicago, IL; 2University of Illinois, Chicago, IL; 3Quincy Medical Group, Quincy, IL; 4University of Illinois College of Medicine, Chicago, IL
Introduction: Inflammatory bowel disease (IBD) patients have a higher risk for colitis-associated dysplasia and neoplasia. Current guidelines recommend the use of dye-based (DCE) or virtual (VCE) chromoendoscopy for enhanced detection and evaluation of abnormal mucosa during surveillance colonoscopy. However, lesion characterization can be difficult in IBD due to morphologically flatter lesions and surrounding inflammation obscuring mucosal pit pattern. Confocal laser endomicroscopy (CLE) is an advanced imaging technique that provides 1,000-fold magnification of the intestinal mucosa and potential for real-time histological diagnosis. CLE can be integrated within the endoscope (eCLE) or via a probe (pCLE). Diagnosing dysplasia in vivo may reduce complications and allow for real-time treatment decisions. Our aim was to determine the diagnostic accuracy of combining DCE and CLE in detecting dysplasia in patients with IBD.
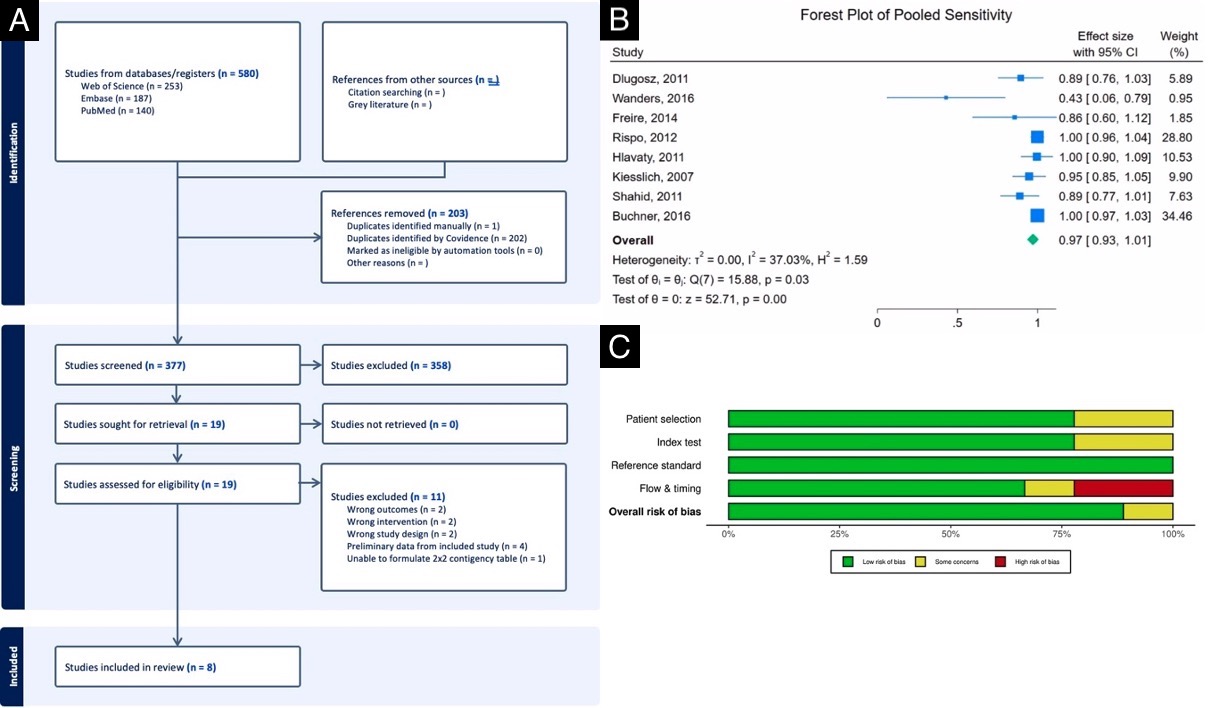
Methods: Per the PRISMA guidelines, PubMed, EMBASE and Web of Science were searched from inception to April 2024 (Figure 1A). The primary outcome was to assess the sensitivity, specificity, and accuracy of DCE-CLE in detecting dysplasia. We performed a bivariate, random effects meta-analysis to analyze the pooled sensitivity, specificity, and accuracy with 95% confidence intervals (CI). A meta-regression was also performed to identify diagnostic differences in pCLE and eCLE. I2 was used to assess heterogeneity. The QUADAS-2 tool was used to assess risk of bias.
Results: Eight studies were included with a total of 410 patients, 500 colonic lesions, 1229 CLE images, and 77 histologically confirmed dysplastic lesions (Table 1). The pooled sensitivity was 97.0% (95% CI: 93.4% - 100%, I2 = 37.03%) (Figure 1B). The pooled specificity was 93.2% (95% CI: 87.6% – 98.7%, I2 = 94.40%) and accuracy 92.9% (95% CI: 87.9% - 97.9%, I2 = 93.14%). pCLE was more sensitive than eCLE (99.2% vs 86.9%, p < 0.05), however less specific (87.4% vs 98.0%, p< 0.001) and accurate (89.5% vs 97.5%, p< 0.001) in dysplasia detection. There was low risk of bias across studies (Figure 1C).
Discussion: Our analysis shows DCE-CLE is a highly effective diagnostic modality for in vivo characterization of dysplasia in patients with IBD. Real-time diagnosis with CLE after lesion detection has the potential to reduce costs and complications related to unnecessary biopsy and polypectomy and enhance real-time treatment decisions. Larger, randomized controlled trials are needed to compare its efficacy with DCE alone and VCE.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael Gianarakis, MD1, Hasan S. Raza, MD2, Omar T. Ahmed, MD1, Elie Ghoulam, MD3, Sandra Naffouj, MD4, Itishree Trivedi, MD, MS2. P4393 - Chromoendoscopy-Guided Endomicroscopy for Dysplasia Surveillance in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2University of Illinois, Chicago, IL; 3Quincy Medical Group, Quincy, IL; 4University of Illinois College of Medicine, Chicago, IL
Introduction: Inflammatory bowel disease (IBD) patients have a higher risk for colitis-associated dysplasia and neoplasia. Current guidelines recommend the use of dye-based (DCE) or virtual (VCE) chromoendoscopy for enhanced detection and evaluation of abnormal mucosa during surveillance colonoscopy. However, lesion characterization can be difficult in IBD due to morphologically flatter lesions and surrounding inflammation obscuring mucosal pit pattern. Confocal laser endomicroscopy (CLE) is an advanced imaging technique that provides 1,000-fold magnification of the intestinal mucosa and potential for real-time histological diagnosis. CLE can be integrated within the endoscope (eCLE) or via a probe (pCLE). Diagnosing dysplasia in vivo may reduce complications and allow for real-time treatment decisions. Our aim was to determine the diagnostic accuracy of combining DCE and CLE in detecting dysplasia in patients with IBD.
Methods: Per the PRISMA guidelines, PubMed, EMBASE and Web of Science were searched from inception to April 2024 (Figure 1A). The primary outcome was to assess the sensitivity, specificity, and accuracy of DCE-CLE in detecting dysplasia. We performed a bivariate, random effects meta-analysis to analyze the pooled sensitivity, specificity, and accuracy with 95% confidence intervals (CI). A meta-regression was also performed to identify diagnostic differences in pCLE and eCLE. I2 was used to assess heterogeneity. The QUADAS-2 tool was used to assess risk of bias.
Results: Eight studies were included with a total of 410 patients, 500 colonic lesions, 1229 CLE images, and 77 histologically confirmed dysplastic lesions (Table 1). The pooled sensitivity was 97.0% (95% CI: 93.4% - 100%, I2 = 37.03%) (Figure 1B). The pooled specificity was 93.2% (95% CI: 87.6% – 98.7%, I2 = 94.40%) and accuracy 92.9% (95% CI: 87.9% - 97.9%, I2 = 93.14%). pCLE was more sensitive than eCLE (99.2% vs 86.9%, p < 0.05), however less specific (87.4% vs 98.0%, p< 0.001) and accurate (89.5% vs 97.5%, p< 0.001) in dysplasia detection. There was low risk of bias across studies (Figure 1C).
Discussion: Our analysis shows DCE-CLE is a highly effective diagnostic modality for in vivo characterization of dysplasia in patients with IBD. Real-time diagnosis with CLE after lesion detection has the potential to reduce costs and complications related to unnecessary biopsy and polypectomy and enhance real-time treatment decisions. Larger, randomized controlled trials are needed to compare its efficacy with DCE alone and VCE.
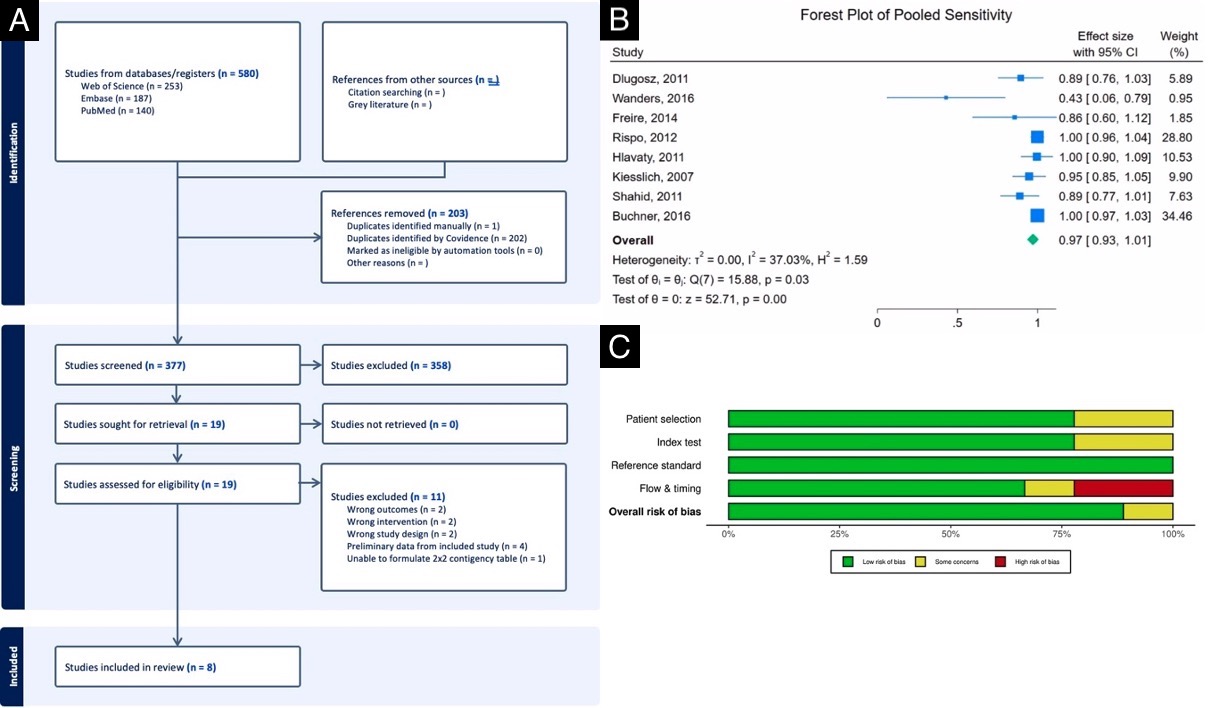
Figure: (A) Flowchart of literature search and study selection per the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines. (B) Forest plot of the pooled sensitivity of DCE-CLE in the detection of colitis-associated dysplasia in IBD patients. (C) Stacked bar chart showing proportion of studies with low, unclear or high risk of bias per the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies) tool.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael Gianarakis indicated no relevant financial relationships.
Hasan Raza indicated no relevant financial relationships.
Omar Ahmed indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Sandra Naffouj indicated no relevant financial relationships.
Itishree Trivedi indicated no relevant financial relationships.
Michael Gianarakis, MD1, Hasan S. Raza, MD2, Omar T. Ahmed, MD1, Elie Ghoulam, MD3, Sandra Naffouj, MD4, Itishree Trivedi, MD, MS2. P4393 - Chromoendoscopy-Guided Endomicroscopy for Dysplasia Surveillance in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

