Tuesday Poster Session
Category: IBD
P4402 - Prevalence and Impact of Zinc Deficiency on Clinical Outcomes in Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Badr Al Bawardy, MD
King Faisal Specialist Hospital and Research Centre
Riyadh, Ar Riyad, Saudi Arabia
Presenting Author(s)
Hend Almuhaya, MD, Raghad Alsalamah, MBBS, Asma Sallam, MBBS, Amgad Alonazy, MBBS, Atheer AlAwwad, BS, Gamal Mohamed, PhD, Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD
King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Inflammatory bowel disease (IBD) can lead to trace elements deficiency such as zinc, which plays a vital role in immune function and tissue repair. The aims of this study were to investigate the prevalence, risk factors and impact of zinc deficiency on clinical outcomes in IBD.
Methods: This is a retrospective, single center study that included patients aged ≥ 14 years with a confirmed diagnosis of IBD [Crohn's disease (CD), ulcerative colitis (UC), pouchitis, IBD-unclassified (IBD-U)] and documented zinc levels. Zinc deficiency was defined as a level < 10.6 umol/L as per our institution’s assay. Primary outcomes were prevalence and predictors of zinc deficiency. Secondary outcomes (assessed over 12 months following initial zinc level) included: rates of IBD-related hospitalizations, emergency room (ER) visits, surgeries, and complications (anemia, small bowel obstruction, new onset perianal disease, intra-abdominal abscess). Univariable and multivariate logistic regression analyses were performed on secondary outcomes.
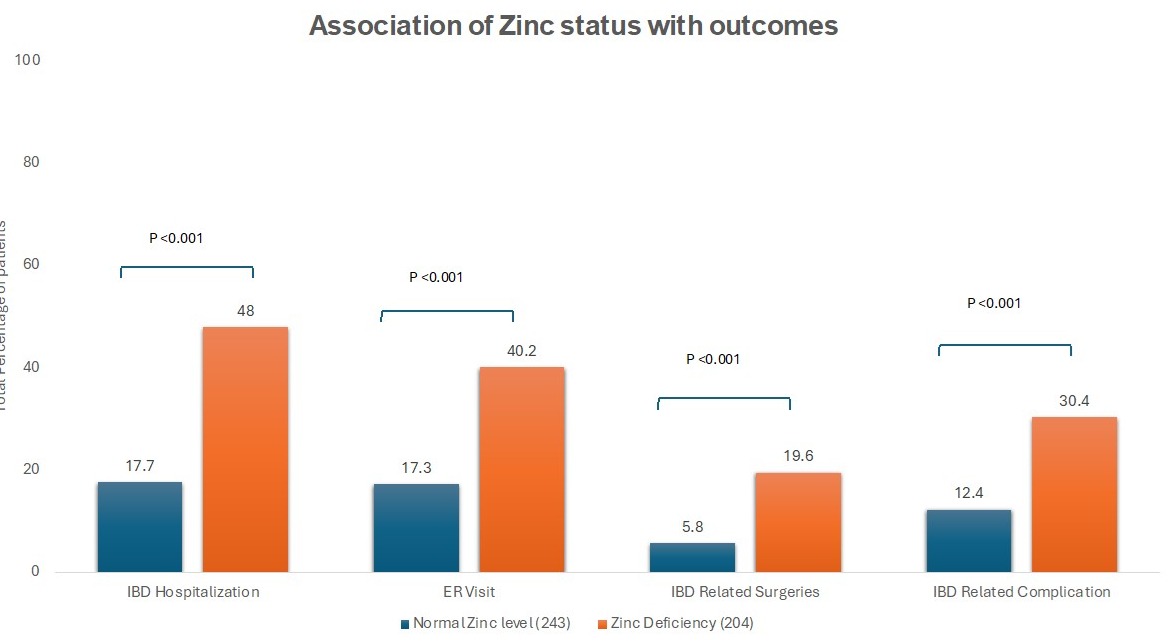
Results: A total of 447 patients (54.4% male; 79.2% CD) were included. Zinc deficiency was noted in 45.6% (83.8% with CD). Patients with zinc deficiency had significantly higher median levels of C-reactive protein (CRP) (p ˂ 0.001), fecal calprotectin (FCP) (p ˂ 0.001) and were more likely to be on corticosteroids (p = 0.04) (Table 1). Zinc-deficient patients had significantly higher rates of IBD-related hospitalizations (48.0% vs. 17.7%), surgeries (19.6% vs. 5.8%), complications (30.4% vs. 12.4%), and ER visits (40.2% vs. 17.3%) (all p < 0.001) (Figure 1). On multivariate analysis, zinc deficiency [odds ratio (OR) 2.42, 95% confidence interval (CI) 1.07-5.48, p = 0.03] and low albumin (OR 9.03, 95% CI 3.38-24.15, p < 0.001) were the only predictors of IBD-related hospitalization while low albumin only predicted ER visits (OR 5.37, 95% CI: 2.13-13.55, p < 0.001). On multivariate analyses, zinc deficiency was significantly associated with IBD-related surgeries (OR 5.23, 95% CI: 1.27-21.45; p = 0.02) and complications (OR 3.98, 95% CI: 1.52-10.41; p = 0.005). CRP and FCP were not significantly associated with any of the secondary outcomes on multivariable analysis.
Discussion: Zinc deficiency was highly prevalent in our cohort of patients with IBD and associated with high inflammatory burden. Zinc deficiency remained associated with unfavorable clinical outcomes after controlling for markers of active inflammation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hend Almuhaya, MD, Raghad Alsalamah, MBBS, Asma Sallam, MBBS, Amgad Alonazy, MBBS, Atheer AlAwwad, BS, Gamal Mohamed, PhD, Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD. P4402 - Prevalence and Impact of Zinc Deficiency on Clinical Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Inflammatory bowel disease (IBD) can lead to trace elements deficiency such as zinc, which plays a vital role in immune function and tissue repair. The aims of this study were to investigate the prevalence, risk factors and impact of zinc deficiency on clinical outcomes in IBD.
Methods: This is a retrospective, single center study that included patients aged ≥ 14 years with a confirmed diagnosis of IBD [Crohn's disease (CD), ulcerative colitis (UC), pouchitis, IBD-unclassified (IBD-U)] and documented zinc levels. Zinc deficiency was defined as a level < 10.6 umol/L as per our institution’s assay. Primary outcomes were prevalence and predictors of zinc deficiency. Secondary outcomes (assessed over 12 months following initial zinc level) included: rates of IBD-related hospitalizations, emergency room (ER) visits, surgeries, and complications (anemia, small bowel obstruction, new onset perianal disease, intra-abdominal abscess). Univariable and multivariate logistic regression analyses were performed on secondary outcomes.
Results: A total of 447 patients (54.4% male; 79.2% CD) were included. Zinc deficiency was noted in 45.6% (83.8% with CD). Patients with zinc deficiency had significantly higher median levels of C-reactive protein (CRP) (p ˂ 0.001), fecal calprotectin (FCP) (p ˂ 0.001) and were more likely to be on corticosteroids (p = 0.04) (Table 1). Zinc-deficient patients had significantly higher rates of IBD-related hospitalizations (48.0% vs. 17.7%), surgeries (19.6% vs. 5.8%), complications (30.4% vs. 12.4%), and ER visits (40.2% vs. 17.3%) (all p < 0.001) (Figure 1). On multivariate analysis, zinc deficiency [odds ratio (OR) 2.42, 95% confidence interval (CI) 1.07-5.48, p = 0.03] and low albumin (OR 9.03, 95% CI 3.38-24.15, p < 0.001) were the only predictors of IBD-related hospitalization while low albumin only predicted ER visits (OR 5.37, 95% CI: 2.13-13.55, p < 0.001). On multivariate analyses, zinc deficiency was significantly associated with IBD-related surgeries (OR 5.23, 95% CI: 1.27-21.45; p = 0.02) and complications (OR 3.98, 95% CI: 1.52-10.41; p = 0.005). CRP and FCP were not significantly associated with any of the secondary outcomes on multivariable analysis.
Discussion: Zinc deficiency was highly prevalent in our cohort of patients with IBD and associated with high inflammatory burden. Zinc deficiency remained associated with unfavorable clinical outcomes after controlling for markers of active inflammation.
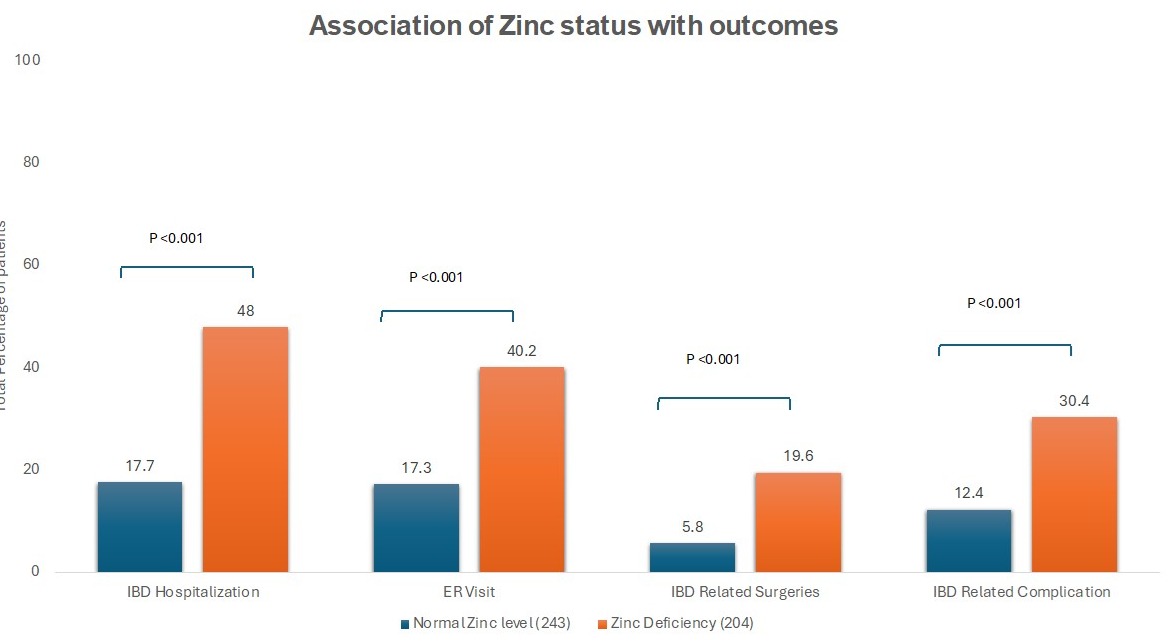
Figure: Figure 1: Secondary Outcomes Stratified by Zinc Level Status
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hend Almuhaya indicated no relevant financial relationships.
Raghad Alsalamah indicated no relevant financial relationships.
Asma Sallam indicated no relevant financial relationships.
Amgad Alonazy indicated no relevant financial relationships.
Atheer AlAwwad indicated no relevant financial relationships.
Gamal Mohamed indicated no relevant financial relationships.
Abdulelah Almutairdi indicated no relevant financial relationships.
Mashary Attamimi indicated no relevant financial relationships.
Badr Al-Bawardy: AbbVie – Consultant, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Takeda – Speakers Bureau.
Hend Almuhaya, MD, Raghad Alsalamah, MBBS, Asma Sallam, MBBS, Amgad Alonazy, MBBS, Atheer AlAwwad, BS, Gamal Mohamed, PhD, Abdulelah Almutairdi, MD, Mashary Attamimi, MD, Badr Al-Bawardy, MD. P4402 - Prevalence and Impact of Zinc Deficiency on Clinical Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

