Tuesday Poster Session
Category: IBD
P4418 - Ecthyma Gangrenosum as a Complication of Immunosuppressive Therapy in Immune-Mediated Colitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lauren A. Lyssy, DO
The University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Lauren A. Lyssy, DO1, Jeremy Polman, DO, MS, MBA2
1The University of Tennessee Health Science Center, Memphis, TN; 2Lenox Hill Hospital, Northwell Health, New York, NY
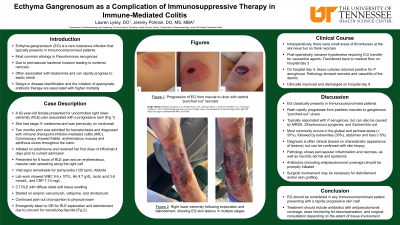
Introduction: Ecthyma gangrenosum (EG) is a rare cutaneous infection that typically presents in immunocompromised patients leading to bacteremia or shock. Pseudomonas aeruginosa is the most common causative bacteria. The primary skin lesions are painless red macules which rapidly progress to pustules then gangrenous ulcers. Delays in disease identification and the initiation of appropriate antibiotic therapy are associated with higher mortality. Here, we present an interesting case of EG in a patient undergoing immunosuppressive therapy for immune checkpoint inhibitor-mediated colitis (IMC).
Case Description/Methods: A 62-year-old female presented with right lower extremity pain and a rash. She had a history of stage IV melanoma with right adrenalectomy. Adjuvant therapy with nivolumab was discontinued 2 months before admission due to hematochezia. She was diagnosed with IMC after undergoing a colonoscopy showing friable, erythematous mucosa and aphthous ulcers throughout the colon. Prednisone was started, followed by the first infusion of infliximab 4 days before admission.
In the ED, she reported 8 hours of right lower extremity pain and a red, macular rash spreading along her right calf. Her initial pulse was 126 bpm without hypotension or fever. Lab work was remarkable for hemoglobin 9.7, lactic acid 3.6, and CRP 7.10. CT right lower extremity showed diffuse distal soft tissue swelling. Empiric vancomycin, cefepime, and clindamycin was given. Due to worsening pain, she was emergently taken to the OR for right lower extremity exploration. Intraoperatively, there were small areas of thromboses at the skin level but no frank necrosis. Biopsies and cultures were obtained. Postoperatively, she became hypotensive and was transferred to the ICU. She improved with empiric antibiotic therapy and was transferred to the medical floor on hospital day 3. Prednisone was also resumed. On hospital day 4, tissue cultures returned positive for P. aeruginosa, and pathology showed necrosis and vasculitis of the dermis. Blood cultures were negative. She continued to improve and was discharged on hospital day 9.
Discussion: EG is an uncommon condition that classically presents in immunocompromised patients with a rash that rapidly progresses from painless macules to gangrenous ulcers. As P. aeruginosa is the most common causative bacteria, it is essential to initiate antibiotics with antipseudomonal coverage when EG is suspected. Surgical involvement may also be necessary depending on the extent of soft tissue infection.
Disclosures:
Lauren A. Lyssy, DO1, Jeremy Polman, DO, MS, MBA2. P4418 - Ecthyma Gangrenosum as a Complication of Immunosuppressive Therapy in Immune-Mediated Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Tennessee Health Science Center, Memphis, TN; 2Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Ecthyma gangrenosum (EG) is a rare cutaneous infection that typically presents in immunocompromised patients leading to bacteremia or shock. Pseudomonas aeruginosa is the most common causative bacteria. The primary skin lesions are painless red macules which rapidly progress to pustules then gangrenous ulcers. Delays in disease identification and the initiation of appropriate antibiotic therapy are associated with higher mortality. Here, we present an interesting case of EG in a patient undergoing immunosuppressive therapy for immune checkpoint inhibitor-mediated colitis (IMC).
Case Description/Methods: A 62-year-old female presented with right lower extremity pain and a rash. She had a history of stage IV melanoma with right adrenalectomy. Adjuvant therapy with nivolumab was discontinued 2 months before admission due to hematochezia. She was diagnosed with IMC after undergoing a colonoscopy showing friable, erythematous mucosa and aphthous ulcers throughout the colon. Prednisone was started, followed by the first infusion of infliximab 4 days before admission.
In the ED, she reported 8 hours of right lower extremity pain and a red, macular rash spreading along her right calf. Her initial pulse was 126 bpm without hypotension or fever. Lab work was remarkable for hemoglobin 9.7, lactic acid 3.6, and CRP 7.10. CT right lower extremity showed diffuse distal soft tissue swelling. Empiric vancomycin, cefepime, and clindamycin was given. Due to worsening pain, she was emergently taken to the OR for right lower extremity exploration. Intraoperatively, there were small areas of thromboses at the skin level but no frank necrosis. Biopsies and cultures were obtained. Postoperatively, she became hypotensive and was transferred to the ICU. She improved with empiric antibiotic therapy and was transferred to the medical floor on hospital day 3. Prednisone was also resumed. On hospital day 4, tissue cultures returned positive for P. aeruginosa, and pathology showed necrosis and vasculitis of the dermis. Blood cultures were negative. She continued to improve and was discharged on hospital day 9.
Discussion: EG is an uncommon condition that classically presents in immunocompromised patients with a rash that rapidly progresses from painless macules to gangrenous ulcers. As P. aeruginosa is the most common causative bacteria, it is essential to initiate antibiotics with antipseudomonal coverage when EG is suspected. Surgical involvement may also be necessary depending on the extent of soft tissue infection.
Disclosures:
Lauren Lyssy indicated no relevant financial relationships.
Jeremy Polman indicated no relevant financial relationships.
Lauren A. Lyssy, DO1, Jeremy Polman, DO, MS, MBA2. P4418 - Ecthyma Gangrenosum as a Complication of Immunosuppressive Therapy in Immune-Mediated Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

