Tuesday Poster Session
Category: IBD
P4422 - Unmasking Intestinal Plasmablastic Lymphoma in an Immunocompetent Crohn’s Disease Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Renieh M. Nabaty, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Award: Presidential Poster Award
Renieh M. Nabaty, MD, Yasmine Hussein Agha, MD, Suraj Suresh, MD
Henry Ford Health, Detroit, MI
Introduction: Plasmablastic lymphoma (PBL) is a rare and aggressive subtype of diffuse large B-cell lymphoma. Originally reported in the oral cavity of immunocompromised HIV patients, it has also been associated with immunosuppression and Epstein-Barr virus (EBV) infection. It commonly manifests in extranodal sites like the GI tract, especially in patients with inflammatory bowel disease (IBD). Diagnosis is challenging due to histological similarities with plasmablastic myeloma, but factors like EBV status and myeloma-defining signs aid in differentiation. We present a rare case of an HIV-negative, immunocompetent, patient with Crohn’s disease post proctocolectomy and end-ileostomy who presented with acute blood loss anemia and was found to have small bowel PBL.
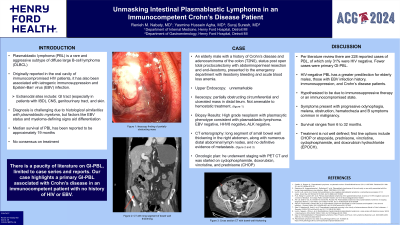
Case Description/Methods: A 75-year-old male with a history of Crohn’s disease and adenocarcinoma of the colon, status post total proctocolectomy with abdominoperineal resection and end-ileostomy, presented with ileostomy bleeding and a significant hemoglobin decrease. He underwent bi-directional endoscopy. Upper endoscopy was unremarkable. Ileoscopy was notable for an obstructing and circumferential ulcerated mass in the distal ileum and severe luminal stenosis. Biopsies of the mass revealed high-grade neoplasm with plasmocytic phenotype, consistent with PBL. CT enterography revealed a long segment of small bowel wall thickening in the right abdomen and numerous distant abdominal lymph nodes, and no evidence of metastasis. Upon follow-up with oncology, he began chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisone.
Discussion: PBL, while primarily associated with HIV patients, has been reported in HIV-negative patients with IBD, and more frequently in Crohn’s disease. This has been hypothesized to be attributed to immunosuppressive therapy or an immunocompromised state. While rare in presentation, reported cases of primary GI-PBL have presented with progressive odynophagia, melena, obstruction, hematochezia, and B symptoms commonly seen in malignancy.
There is a paucity of literature on GI-PBL, limited to case series and reports. Our case highlights a primary GI-PBL associated with Crohn’s disease in an immunocompetent patient with no history of HIV or EBV. To date, a treatment regimen has not been well defined. Despite treatment advancements, PBL patients have an average survival of 19 months. Thus, it is vital to consider GI-PBL on the differential and continue research on this rare and diagnostically challenging malignancy.
Disclosures:
Renieh M. Nabaty, MD, Yasmine Hussein Agha, MD, Suraj Suresh, MD. P4422 - Unmasking Intestinal Plasmablastic Lymphoma in an Immunocompetent Crohn’s Disease Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Renieh M. Nabaty, MD, Yasmine Hussein Agha, MD, Suraj Suresh, MD
Henry Ford Health, Detroit, MI
Introduction: Plasmablastic lymphoma (PBL) is a rare and aggressive subtype of diffuse large B-cell lymphoma. Originally reported in the oral cavity of immunocompromised HIV patients, it has also been associated with immunosuppression and Epstein-Barr virus (EBV) infection. It commonly manifests in extranodal sites like the GI tract, especially in patients with inflammatory bowel disease (IBD). Diagnosis is challenging due to histological similarities with plasmablastic myeloma, but factors like EBV status and myeloma-defining signs aid in differentiation. We present a rare case of an HIV-negative, immunocompetent, patient with Crohn’s disease post proctocolectomy and end-ileostomy who presented with acute blood loss anemia and was found to have small bowel PBL.
Case Description/Methods: A 75-year-old male with a history of Crohn’s disease and adenocarcinoma of the colon, status post total proctocolectomy with abdominoperineal resection and end-ileostomy, presented with ileostomy bleeding and a significant hemoglobin decrease. He underwent bi-directional endoscopy. Upper endoscopy was unremarkable. Ileoscopy was notable for an obstructing and circumferential ulcerated mass in the distal ileum and severe luminal stenosis. Biopsies of the mass revealed high-grade neoplasm with plasmocytic phenotype, consistent with PBL. CT enterography revealed a long segment of small bowel wall thickening in the right abdomen and numerous distant abdominal lymph nodes, and no evidence of metastasis. Upon follow-up with oncology, he began chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisone.
Discussion: PBL, while primarily associated with HIV patients, has been reported in HIV-negative patients with IBD, and more frequently in Crohn’s disease. This has been hypothesized to be attributed to immunosuppressive therapy or an immunocompromised state. While rare in presentation, reported cases of primary GI-PBL have presented with progressive odynophagia, melena, obstruction, hematochezia, and B symptoms commonly seen in malignancy.
There is a paucity of literature on GI-PBL, limited to case series and reports. Our case highlights a primary GI-PBL associated with Crohn’s disease in an immunocompetent patient with no history of HIV or EBV. To date, a treatment regimen has not been well defined. Despite treatment advancements, PBL patients have an average survival of 19 months. Thus, it is vital to consider GI-PBL on the differential and continue research on this rare and diagnostically challenging malignancy.
Disclosures:
Renieh Nabaty indicated no relevant financial relationships.
Yasmine Hussein Agha indicated no relevant financial relationships.
Suraj Suresh indicated no relevant financial relationships.
Renieh M. Nabaty, MD, Yasmine Hussein Agha, MD, Suraj Suresh, MD. P4422 - Unmasking Intestinal Plasmablastic Lymphoma in an Immunocompetent Crohn’s Disease Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

