Tuesday Poster Session
Category: Interventional Endoscopy
P4455 - Prone ERCP is Associated with Higher Successful Cannulation Rates Compared to Supine ERCP: A Systematic Review and Meta-analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Asaiel Makahleh, MD
East Tennessee State University
Johnson City, TN
Presenting Author(s)
Rasheed Musa, MD1, Asaiel Makahleh, MD1, Ahmad Alnasarat, MD2, Mohammad N. Kloub, MD3, Sharifeh Almasaid, MD4, Mohammad Darweesh, MD1, Rashid Abdel-razeq, MD5, Hamza Asif, MD6, Mark Young, MD1
1East Tennessee State University, Johnson City, TN; 2DMC Sinai-Grace Hospital, Farmington Hills, MI; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4SUNY Upstate Medical University, Johnson City, TN; 5Cleveland Clinic Foundation, Cleveland, OH; 6Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is a widely utilized procedure for diagnosing and treating pancreaticobiliary disorders. The optimal patient positioning during ERCP, whether supine or prone, remains a subject of debate. This meta-analysis aims to systematically compare the clinical outcomes associated with supine and prone ERCP positions.
Methods: We conducted a systematic review and search of PubMed/MEDLINE, EMBASE, SCOPUS, and Cochrane databases to identify studies published up to the knowledge cutoff date in 2023. Inclusion criteria encompassed randomized controlled trials, cohort studies, and case-control studies directly comparing supine and prone ERCP positions. Statistical analyses were performed using random-effects models to calculate pooled odds ratios (OR) and weighted mean differences (WMD) with 95% confidence intervals (CI) for dichotomous and continuous outcomes, respectively.
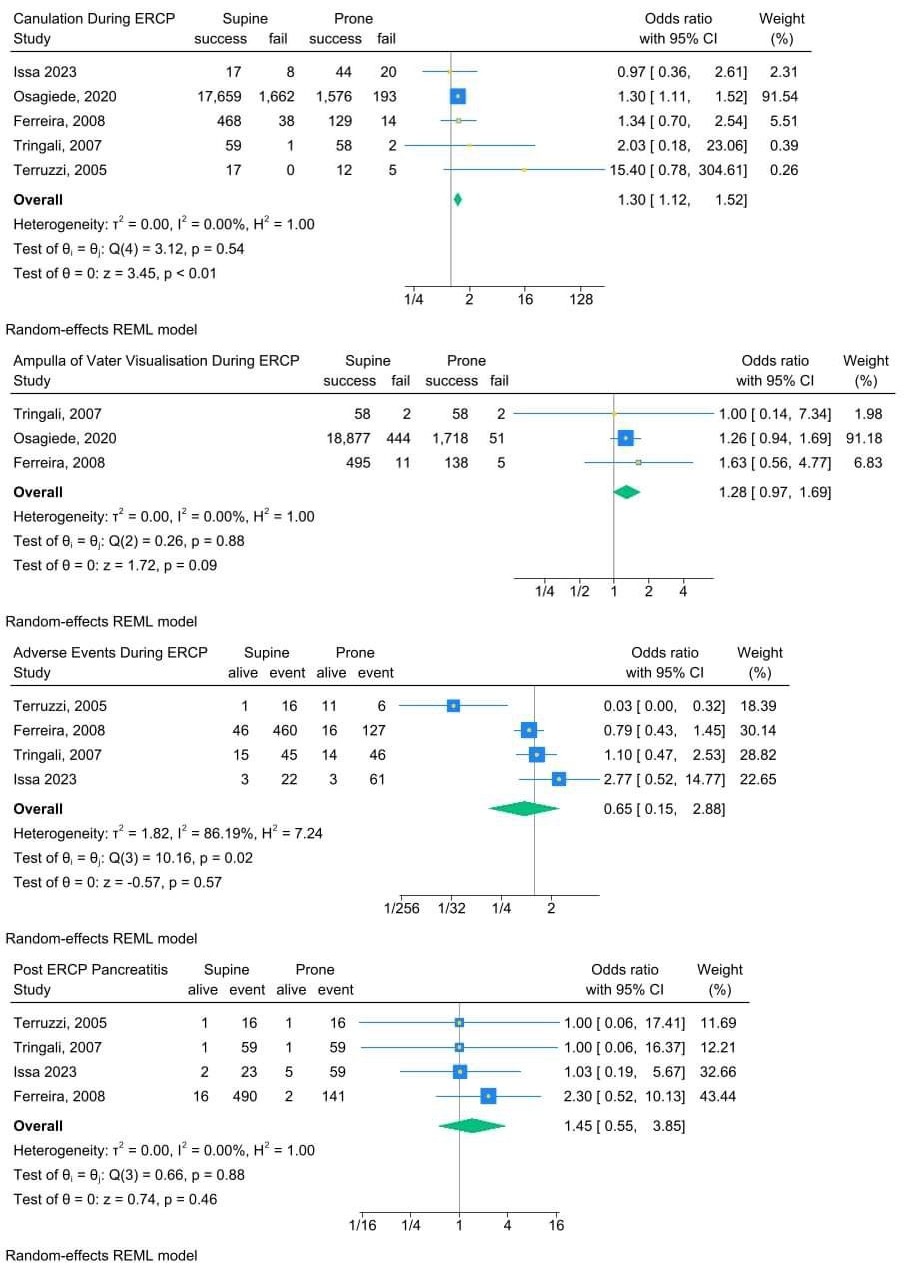
Results: A total of 5 studies (21,982 patients) were included in the meta-analysis, comprising a combined sample size of participants. The primary outcome assessed included a successful cannulation rate. Secondary outcomes comprised ampulla of Vater visualization, total adverse events rate, and post-ERCP pancreatitis rate. The meta-analysis revealed that prone ERCP was associated with a higher successful cannulation rate compared to supine ERCP with OR 1.30 [95% CI 1.12 to 1.52] for the prone position. No significant difference was detected between the supine and prone position when comparing the ampulla of Vater visualization, total adverse events rate, and post-ERCP pancreatitis rate with corresponding OR 1.28 [95% CI 0.97 to 1.69], 0.65 [95% CI 0.15 to 2.88], 1.45 [95% CI 0.55 to 3.85], respectively.
Discussion: This meta-analysis provides a comprehensive synthesis of current evidence comparing supine and prone ERCP positions. The findings suggest that prone ERCP may offer advantages in terms of procedural success rates, namely cannulation rate. However, individual patient characteristics and procedural indications should be considered when determining the optimal positioning strategy. Further well-designed prospective studies are warranted to validate these findings and guide clinical practice.
Disclosures:
Rasheed Musa, MD1, Asaiel Makahleh, MD1, Ahmad Alnasarat, MD2, Mohammad N. Kloub, MD3, Sharifeh Almasaid, MD4, Mohammad Darweesh, MD1, Rashid Abdel-razeq, MD5, Hamza Asif, MD6, Mark Young, MD1. P4455 - Prone ERCP is Associated with Higher Successful Cannulation Rates Compared to Supine ERCP: A Systematic Review and Meta-analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1East Tennessee State University, Johnson City, TN; 2DMC Sinai-Grace Hospital, Farmington Hills, MI; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4SUNY Upstate Medical University, Johnson City, TN; 5Cleveland Clinic Foundation, Cleveland, OH; 6Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is a widely utilized procedure for diagnosing and treating pancreaticobiliary disorders. The optimal patient positioning during ERCP, whether supine or prone, remains a subject of debate. This meta-analysis aims to systematically compare the clinical outcomes associated with supine and prone ERCP positions.
Methods: We conducted a systematic review and search of PubMed/MEDLINE, EMBASE, SCOPUS, and Cochrane databases to identify studies published up to the knowledge cutoff date in 2023. Inclusion criteria encompassed randomized controlled trials, cohort studies, and case-control studies directly comparing supine and prone ERCP positions. Statistical analyses were performed using random-effects models to calculate pooled odds ratios (OR) and weighted mean differences (WMD) with 95% confidence intervals (CI) for dichotomous and continuous outcomes, respectively.
Results: A total of 5 studies (21,982 patients) were included in the meta-analysis, comprising a combined sample size of participants. The primary outcome assessed included a successful cannulation rate. Secondary outcomes comprised ampulla of Vater visualization, total adverse events rate, and post-ERCP pancreatitis rate. The meta-analysis revealed that prone ERCP was associated with a higher successful cannulation rate compared to supine ERCP with OR 1.30 [95% CI 1.12 to 1.52] for the prone position. No significant difference was detected between the supine and prone position when comparing the ampulla of Vater visualization, total adverse events rate, and post-ERCP pancreatitis rate with corresponding OR 1.28 [95% CI 0.97 to 1.69], 0.65 [95% CI 0.15 to 2.88], 1.45 [95% CI 0.55 to 3.85], respectively.
Discussion: This meta-analysis provides a comprehensive synthesis of current evidence comparing supine and prone ERCP positions. The findings suggest that prone ERCP may offer advantages in terms of procedural success rates, namely cannulation rate. However, individual patient characteristics and procedural indications should be considered when determining the optimal positioning strategy. Further well-designed prospective studies are warranted to validate these findings and guide clinical practice.
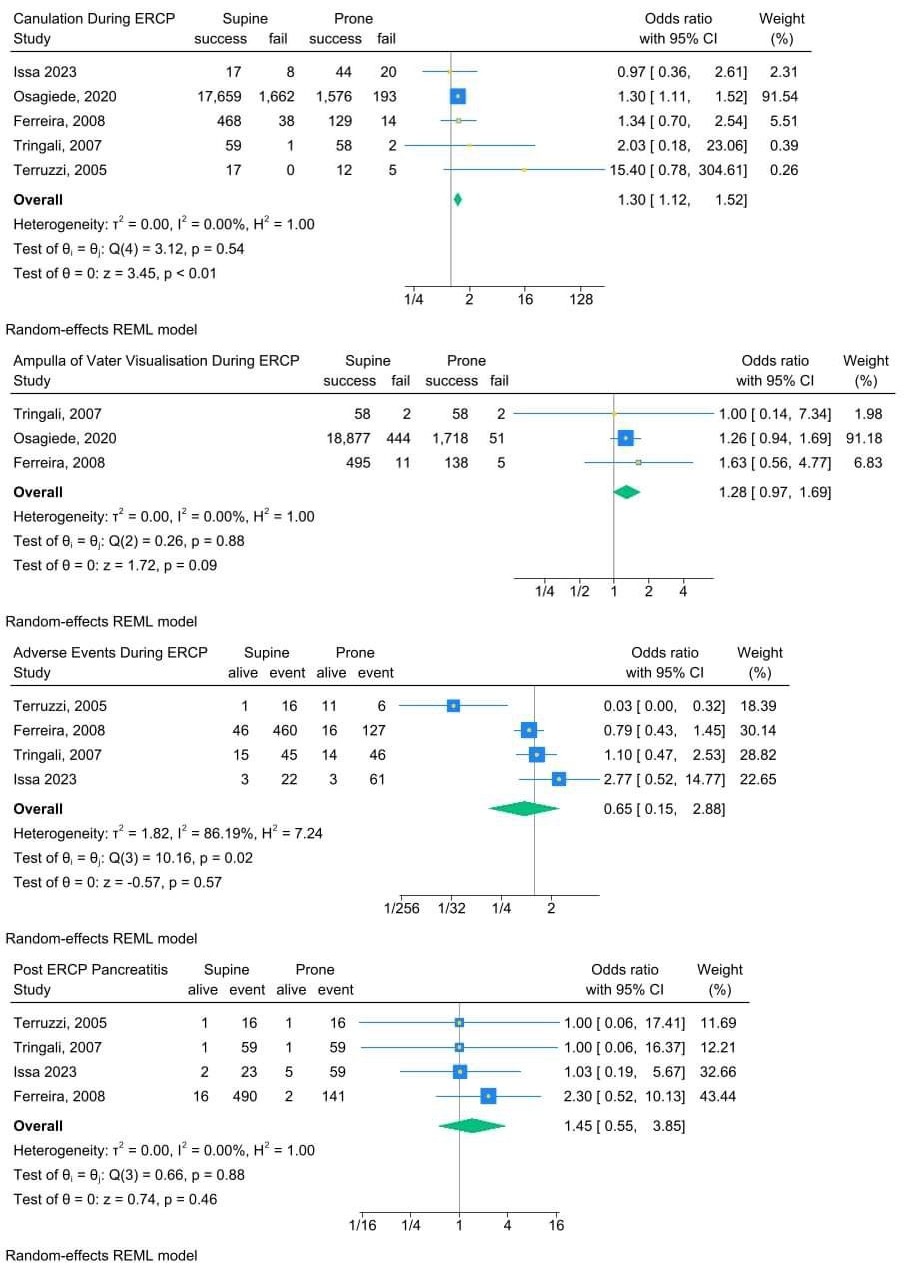
Figure: Meta-analysis results
Disclosures:
Rasheed Musa indicated no relevant financial relationships.
Asaiel Makahleh indicated no relevant financial relationships.
Ahmad Alnasarat indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Sharifeh Almasaid indicated no relevant financial relationships.
Mohammad Darweesh indicated no relevant financial relationships.
Rashid Abdel-razeq indicated no relevant financial relationships.
Hamza Asif indicated no relevant financial relationships.
Mark Young indicated no relevant financial relationships.
Rasheed Musa, MD1, Asaiel Makahleh, MD1, Ahmad Alnasarat, MD2, Mohammad N. Kloub, MD3, Sharifeh Almasaid, MD4, Mohammad Darweesh, MD1, Rashid Abdel-razeq, MD5, Hamza Asif, MD6, Mark Young, MD1. P4455 - Prone ERCP is Associated with Higher Successful Cannulation Rates Compared to Supine ERCP: A Systematic Review and Meta-analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
