Tuesday Poster Session
Category: Interventional Endoscopy
P4468 - Endoscopic Mucosal Resection (EMR) vs Endoscopic Submucosal Dissection (ESD) for Early Gastric Cancer: An Updated Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Amna Iqbal, MD
University of Toledo Medical Center
Toledo, OH
Presenting Author(s)
Amna Iqbal, MD1, Zohaib Ahmed, MD1, Rehmat Ullah Awan, MD2, Manesh Kumar Gangwani, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Umar Hayat, MD6, Vishali Moond, MD7, Babu Mohan, MD8, Sahithi Chinnam, DO3, Sana Rabeeah, MD3, Yaseen Alastal, MD1, Shailendra Singh, MD2
1University of Toledo Medical Center, Toledo, OH; 2West Virginia University, Morgantown, WV; 3University of Toledo, Toledo, OH; 4The University of Kansas School of Medicine, Kansas City, KS; 5ECU Health Medical Center, Greenville, NC; 6Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 7Saint Peter's University Hospital, New Brunswick, NJ; 8Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic submucosal dissection (ESD) has been developed to overcome the limitations of endoscopic mucosal resection (EMR). The role of EMR cannot be understated, especially in small lesions. This study compares the efficacy and safety of ESD and EMR in the treatment of early gastric cancer (EGC) based on lesion size.
Methods: Studies investigating the safety and efficacy of ESD and EMR for EGC were searched from the databases of PubMed, Web of Science, EMBASE and the Cochrane Library. Primary end points included en bloc resection, procedure time and local recurrence. Secondary end points included perforation, bleeding, complete and curative resection rates. Random-effects model was used for statistical analysis.
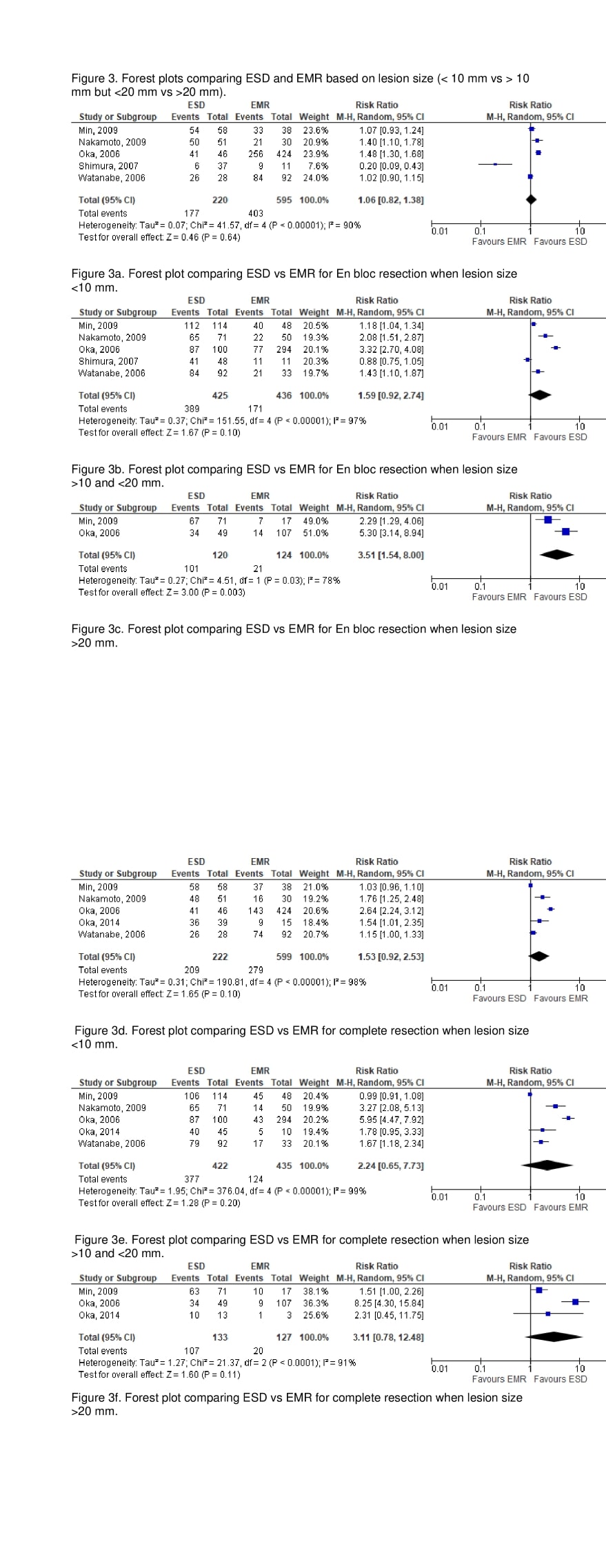
Results: Twenty-three studies were included in the meta-analysis. ESD had significantly higher en bloc [Risk Ratio (RR): 1.51, CI: 1.20-1.91, P = < 0.00001, I 2 = 99%], longer procedure duration (RR:1.20, CI: 0.43-1.97, P = < 0.00001, I 2 = 98%) and lower recurrence rate (RR:0.28, CI: 0.14-0.57, P = 0.0004, I 2 = 43%). ESD is associated with higher complete resection and curative resection rates compared to EMR. However, post operative bleeding and perforation rates for ESD were significantly higher than those for EMR. When compared for lesion size, ESD is associated with higher EN bloc resection rate compared to EMR when lesions are >20 mm. ESD is similar to EMR for complete resection regardless of lesion size. Meta-regression did not reveal statistically significant study-level relationships between study differences in any of the covariates that could account for the greater rates of En bloc resection, procedure duration and lower rates of local recurrence with ESD procedures.
Discussion: ESD is superior to EMR in the treatment of EGC with higher en bloc, curative and complete resection rates and by obviously lower local recurrence rate. Nevertheless, the selection of ESD or EMR should take lesion size into consideration. EMR is appropriate when lesion size <20 mm, ESD is superior when lesion size >20 mm. More evidence is needed to confirm the current findings.
Disclosures:
Amna Iqbal, MD1, Zohaib Ahmed, MD1, Rehmat Ullah Awan, MD2, Manesh Kumar Gangwani, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Umar Hayat, MD6, Vishali Moond, MD7, Babu Mohan, MD8, Sahithi Chinnam, DO3, Sana Rabeeah, MD3, Yaseen Alastal, MD1, Shailendra Singh, MD2. P4468 - Endoscopic Mucosal Resection (EMR) vs Endoscopic Submucosal Dissection (ESD) for Early Gastric Cancer: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Toledo Medical Center, Toledo, OH; 2West Virginia University, Morgantown, WV; 3University of Toledo, Toledo, OH; 4The University of Kansas School of Medicine, Kansas City, KS; 5ECU Health Medical Center, Greenville, NC; 6Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 7Saint Peter's University Hospital, New Brunswick, NJ; 8Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic submucosal dissection (ESD) has been developed to overcome the limitations of endoscopic mucosal resection (EMR). The role of EMR cannot be understated, especially in small lesions. This study compares the efficacy and safety of ESD and EMR in the treatment of early gastric cancer (EGC) based on lesion size.
Methods: Studies investigating the safety and efficacy of ESD and EMR for EGC were searched from the databases of PubMed, Web of Science, EMBASE and the Cochrane Library. Primary end points included en bloc resection, procedure time and local recurrence. Secondary end points included perforation, bleeding, complete and curative resection rates. Random-effects model was used for statistical analysis.
Results: Twenty-three studies were included in the meta-analysis. ESD had significantly higher en bloc [Risk Ratio (RR): 1.51, CI: 1.20-1.91, P = < 0.00001, I 2 = 99%], longer procedure duration (RR:1.20, CI: 0.43-1.97, P = < 0.00001, I 2 = 98%) and lower recurrence rate (RR:0.28, CI: 0.14-0.57, P = 0.0004, I 2 = 43%). ESD is associated with higher complete resection and curative resection rates compared to EMR. However, post operative bleeding and perforation rates for ESD were significantly higher than those for EMR. When compared for lesion size, ESD is associated with higher EN bloc resection rate compared to EMR when lesions are >20 mm. ESD is similar to EMR for complete resection regardless of lesion size. Meta-regression did not reveal statistically significant study-level relationships between study differences in any of the covariates that could account for the greater rates of En bloc resection, procedure duration and lower rates of local recurrence with ESD procedures.
Discussion: ESD is superior to EMR in the treatment of EGC with higher en bloc, curative and complete resection rates and by obviously lower local recurrence rate. Nevertheless, the selection of ESD or EMR should take lesion size into consideration. EMR is appropriate when lesion size <20 mm, ESD is superior when lesion size >20 mm. More evidence is needed to confirm the current findings.
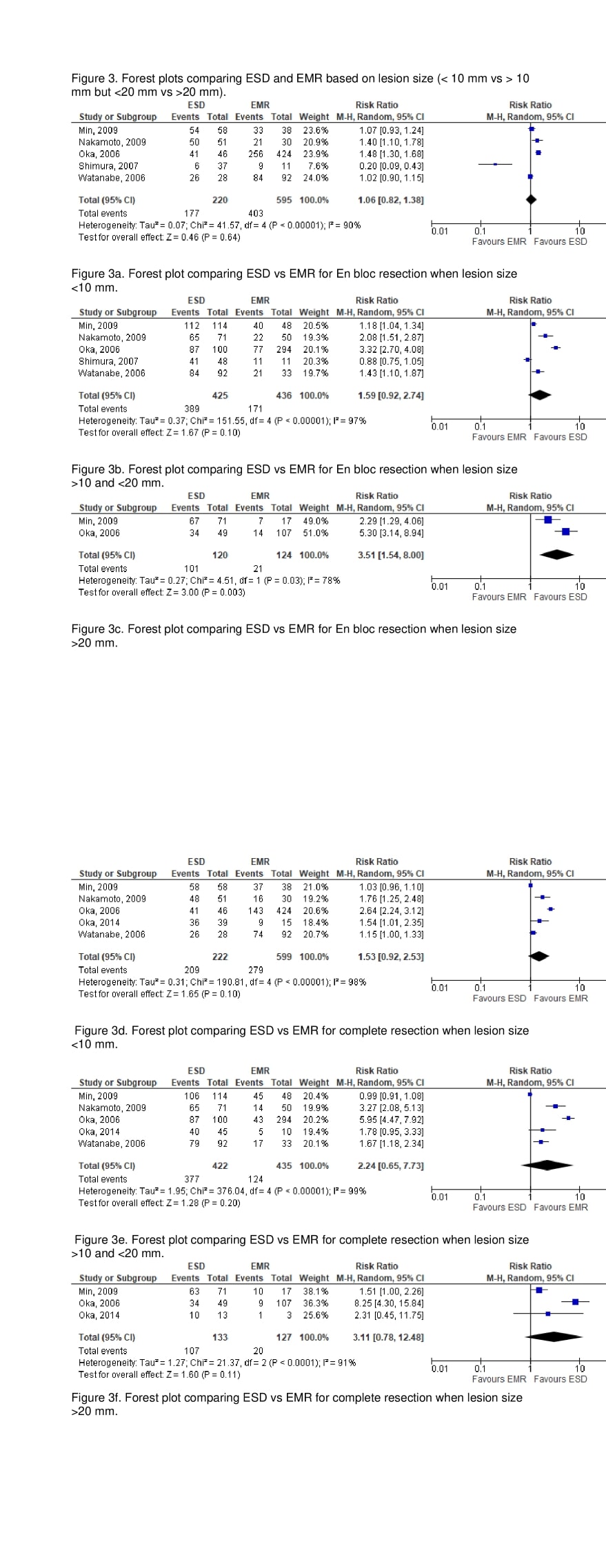
Figure: Figure 3 comparing ESD and EMR for EGC resection based on lesion size
Disclosures:
Amna Iqbal indicated no relevant financial relationships.
Zohaib Ahmed indicated no relevant financial relationships.
Rehmat Ullah Awan indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Sahithi Chinnam indicated no relevant financial relationships.
Sana Rabeeah indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Shailendra Singh: Apollo Endosurgery – Consultant. Boston Scientific – Consultant. Fujifilm Endoscopy – Consultant.
Amna Iqbal, MD1, Zohaib Ahmed, MD1, Rehmat Ullah Awan, MD2, Manesh Kumar Gangwani, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Umar Hayat, MD6, Vishali Moond, MD7, Babu Mohan, MD8, Sahithi Chinnam, DO3, Sana Rabeeah, MD3, Yaseen Alastal, MD1, Shailendra Singh, MD2. P4468 - Endoscopic Mucosal Resection (EMR) vs Endoscopic Submucosal Dissection (ESD) for Early Gastric Cancer: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
