Tuesday Poster Session
Category: Interventional Endoscopy
P4470 - Impact of Statin Use on Post-ERCP Complications: A U.S. Cohort Propensity-Matched Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Alsabbagh Alchirazi, MD
Aurora Healthcare
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Ahmad Najdat Bazarbashi, MD5
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4Cleveland Clinic, Cleveland, OH; 5Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is essential for diagnosing and treating pancreatic and biliary diseases. However, it carries several risks and complications, such as pancreatitis and aspiration. Statins, besides their well-known lipid-lowering effects, exhibit significant anti-inflammatory and immunomodulatory properties. Despite their potential, data on the impact of statins on ERCP outcomes are limited. This study utilizes a large database to investigate how statins might improve the safety and outcomes of ERCP.
Methods: This retrospective cohort study using the TriNetX database included patients who underwent ERCP and received statins (fluvastatin, pitavastatin, simvastatin, atorvastatin, pravastatin, rosuvastatin, lovastatin) between 2010-2024. This cohort was matched with non-statin users by age, demographics, Charlson comorbidity index, and aspirin use using 1:1 propensity score matching (PSM). Primary outcomes included the risk of post-ERCP pancreatitis (PEP), gastrointestinal (GI) bleeding, GI perforation, systemic complications (critical care services, acute kidney injury, intubation, dialysis, shock, acute hypoxic respiratory failure), aspiration pneumonia, intubation, and all-cause mortality within 30 days after ERCP.
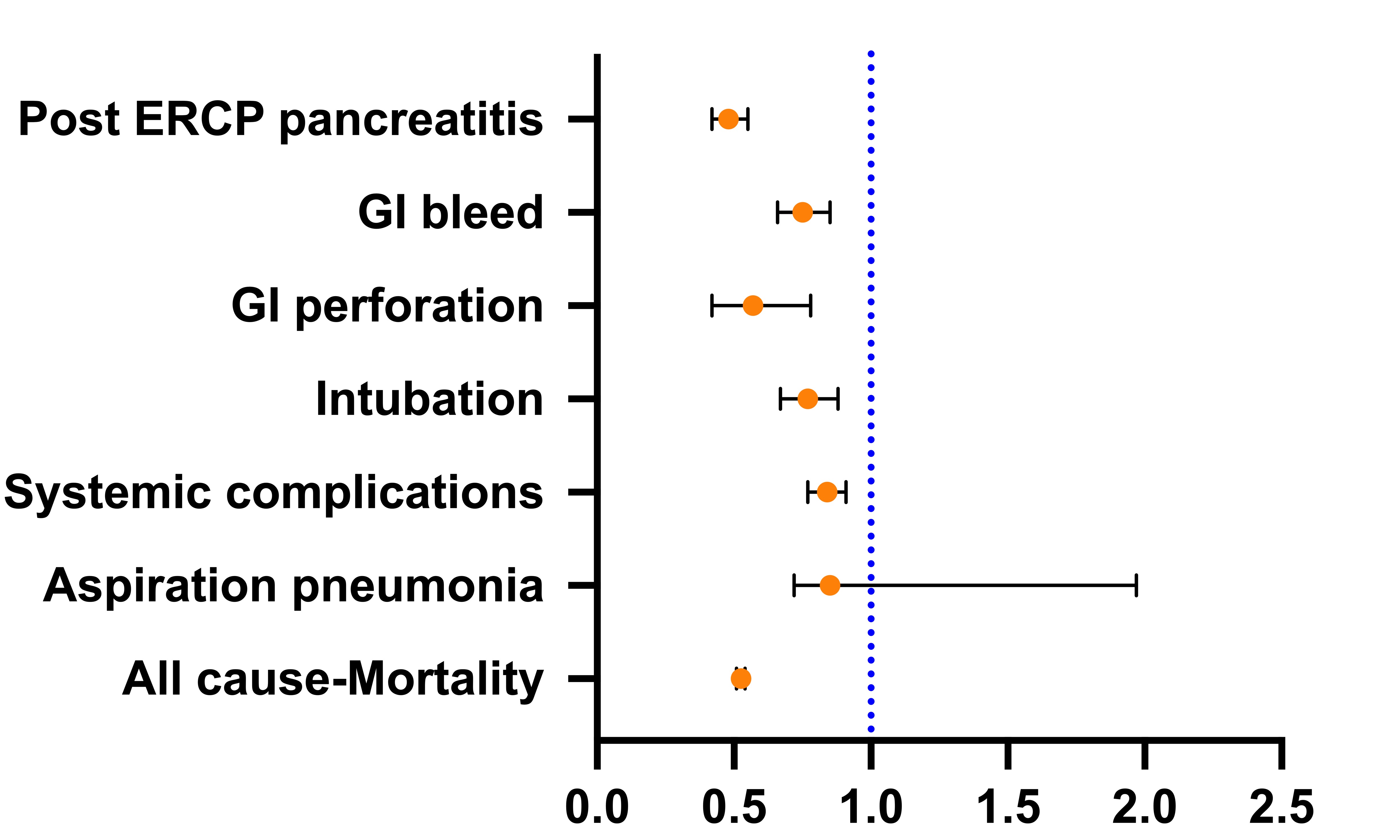
Results: General characteristics in Table 1. After PSM, we had 37,826 patients in both groups. Patients who were on statins and underwent ERCP had a lower risk of intubation (HR 0.77, 95% CI [0.67-0.88]), PEP (0.48, [0.42-0.55]), GI bleeding (0.75, [0.66-0.85]), GI perforation (0.57, [0.42-0.78]), systemic complications (0.84, [0.77-0.91]), and all-cause mortality (0.51, [0.47-0.54]) within 30 days of the ERCP. However, there was no significant difference in the development of aspiration pneumonia (0.85, [0.72-1.97]), Figure 1.
Discussion: Our study suggests a potential prophylactic role for statin use before ERCP, highlighting its anti-inflammatory effects. Statins may reduce the risk of intubation, PEP, GI bleeding & perforation, systemic complications, and all-cause mortality within 30 days of ERCP. However, there was no difference in aspiration pneumonia. Given the anti-inflammatory properties of statins, they might contribute to these protective effects. To further investigate and enhance patient outcomes, randomized controlled trials are essential. These trials could provide more definitive evidence and help establish statins as a standard pre-procedural care option for ERCP patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Ahmad Najdat Bazarbashi, MD5. P4470 - Impact of Statin Use on Post-ERCP Complications: A U.S. Cohort Propensity-Matched Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4Cleveland Clinic, Cleveland, OH; 5Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic Retrograde Cholangiopancreatography (ERCP) is essential for diagnosing and treating pancreatic and biliary diseases. However, it carries several risks and complications, such as pancreatitis and aspiration. Statins, besides their well-known lipid-lowering effects, exhibit significant anti-inflammatory and immunomodulatory properties. Despite their potential, data on the impact of statins on ERCP outcomes are limited. This study utilizes a large database to investigate how statins might improve the safety and outcomes of ERCP.
Methods: This retrospective cohort study using the TriNetX database included patients who underwent ERCP and received statins (fluvastatin, pitavastatin, simvastatin, atorvastatin, pravastatin, rosuvastatin, lovastatin) between 2010-2024. This cohort was matched with non-statin users by age, demographics, Charlson comorbidity index, and aspirin use using 1:1 propensity score matching (PSM). Primary outcomes included the risk of post-ERCP pancreatitis (PEP), gastrointestinal (GI) bleeding, GI perforation, systemic complications (critical care services, acute kidney injury, intubation, dialysis, shock, acute hypoxic respiratory failure), aspiration pneumonia, intubation, and all-cause mortality within 30 days after ERCP.
Results: General characteristics in Table 1. After PSM, we had 37,826 patients in both groups. Patients who were on statins and underwent ERCP had a lower risk of intubation (HR 0.77, 95% CI [0.67-0.88]), PEP (0.48, [0.42-0.55]), GI bleeding (0.75, [0.66-0.85]), GI perforation (0.57, [0.42-0.78]), systemic complications (0.84, [0.77-0.91]), and all-cause mortality (0.51, [0.47-0.54]) within 30 days of the ERCP. However, there was no significant difference in the development of aspiration pneumonia (0.85, [0.72-1.97]), Figure 1.
Discussion: Our study suggests a potential prophylactic role for statin use before ERCP, highlighting its anti-inflammatory effects. Statins may reduce the risk of intubation, PEP, GI bleeding & perforation, systemic complications, and all-cause mortality within 30 days of ERCP. However, there was no difference in aspiration pneumonia. Given the anti-inflammatory properties of statins, they might contribute to these protective effects. To further investigate and enhance patient outcomes, randomized controlled trials are essential. These trials could provide more definitive evidence and help establish statins as a standard pre-procedural care option for ERCP patients.
Figure: Clinical outcomes for propensity-matched of patients who were on statin vs not that underwent endoscopic retrograde cholangiopancreatography
in the United States
in the United States
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Ahmed El Telbany indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Ahmad Najdat Bazarbashi indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Ahmad Najdat Bazarbashi, MD5. P4470 - Impact of Statin Use on Post-ERCP Complications: A U.S. Cohort Propensity-Matched Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
