Tuesday Poster Session
Category: Interventional Endoscopy
P4471 - Glucagon-Like Peptide-1 Receptor Agonists Are Not Associated With Higher Risk of Intubation or Aspiration Pneumonia in Patients Who Underwent ERCP: A National Cohort Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Alsabbagh Alchirazi, MD
Aurora Healthcare
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Marina Kim, MD2, Tarek Sawas, MD4
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4UT Southwestern, Coppell, TX
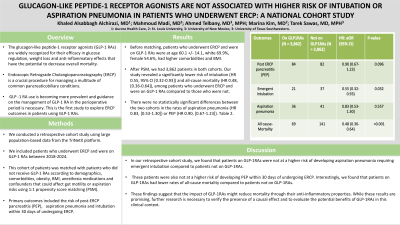
Introduction: The glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are widely recognized for their efficacy in glucose regulation, weight loss and anti-inflammatory effects that have the potential to decrease overall mortality. Endoscopic Retrograde Cholangiopancreatography (ERCP) is a crucial procedure for managing a multitude of common pancreaticobiliary conditions. GLP -1 RA use is becoming more prevalent and guidance on the management of GLP-1 RA in the perioperative period is necessary. This is the first study to explore ERCP outcomes in patients using GLP-1 RAs.
Methods: We conducted a retrospective cohort study using large population-based data from the TriNetX platform. We included patients who underwent ERCP and were on GLP-1 RAs between 2018-2024. This cohort of patients was matched with patients who did not receive GLP-1 RAs according to demographics, comorbidities, obesity, BMI, anesthesia medications and confounders that could affect gut motility or aspiration risks using 1:1 propensity score matching (PSM). Primary outcomes included the risk of post-ERCP pancreatitis (PEP), aspiration pneumonia and intubation within 30 days of undergoing ERCP
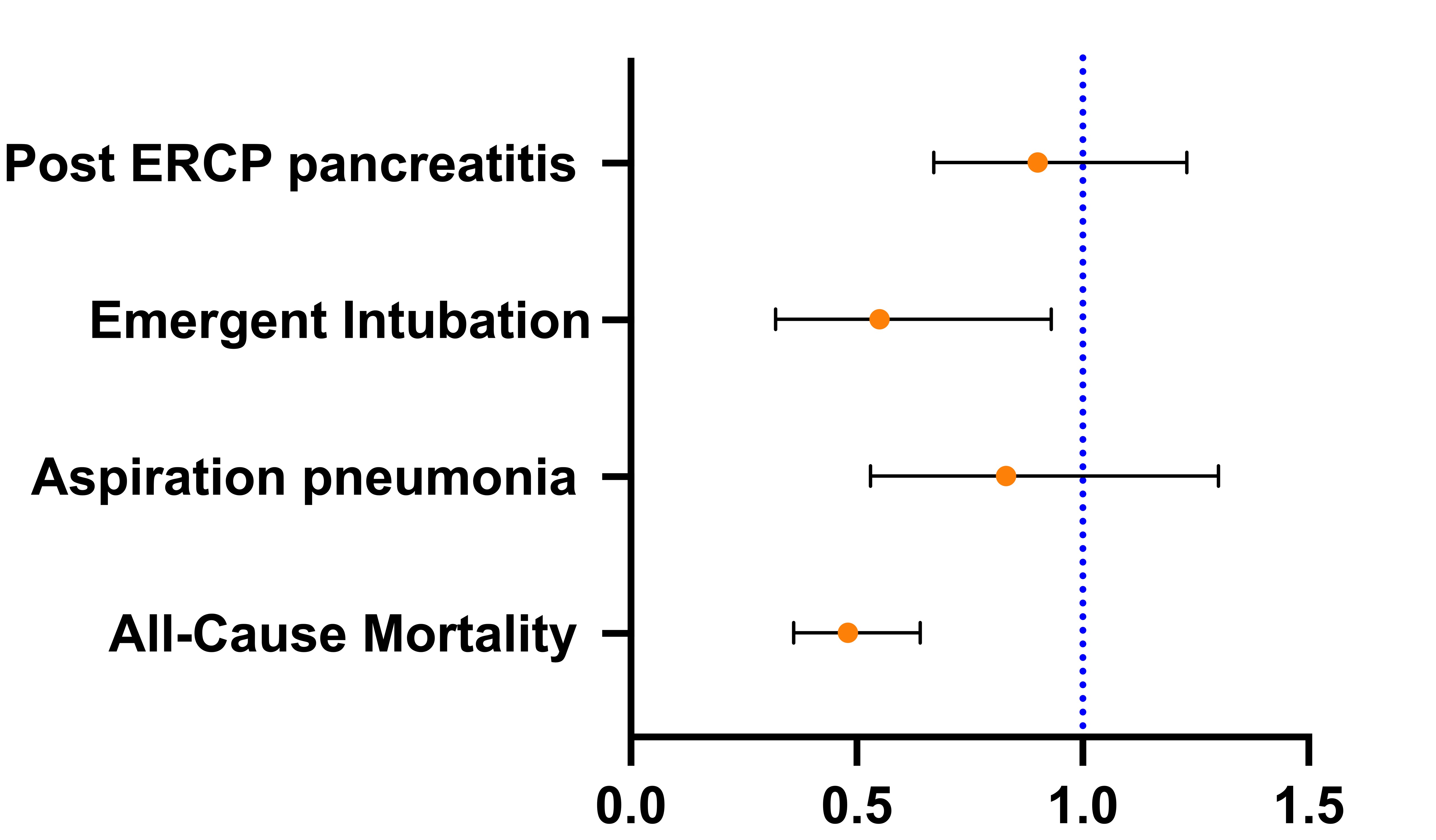
Results: Before matching, patients who underwent ERCP and were on GLP-1 RAs were at age 60.1 +/- 14.1, white 69.9%, female 54.6%, had higher comorbidities and BMI, table 1. After PSM, we had 3,862 patients in both cohorts. Our study revealed a significantly lower risk of intubation (HR 0.55, 95% CI [0.32-0.93]) and all-cause mortality (HR 0.48, [0.36-0.64]), among patients who underwent ERCP and were on GLP-1 RAs compared to those who were not. There were no statistically significant differences between the two cohorts in the rates of aspiration pneumonia (HR 0.83, [0.53-1.30]) or PEP (HR 0.90, [0.67-1.23]). Figure 1.
Discussion: In our retrospective cohort study, we found that patients on GLP-1RAs were not at a higher risk of developing aspiration pneumonia or requiring emergent intubation compared to patients not on GLP-1RAs. These patients were also not at a higher risk of developing PEP within 30 days of undergoing ERCP. Interestingly, we found that patients on GLP-1RAs had lower rates of all-cause mortality compared to patients not on GLP-1RAs. These findings suggest that the impact of GLP-1RAs might reduce mortality through their anti-inflammatory properties. While these results are promising, further research is necessary to verify the presence of a causal effect and to evaluate the potential benefits of GLP-1RAs in this clinical context.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Marina Kim, MD2, Tarek Sawas, MD4. P4471 - Glucagon-Like Peptide-1 Receptor Agonists Are Not Associated With Higher Risk of Intubation or Aspiration Pneumonia in Patients Who Underwent ERCP: A National Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4UT Southwestern, Coppell, TX
Introduction: The glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are widely recognized for their efficacy in glucose regulation, weight loss and anti-inflammatory effects that have the potential to decrease overall mortality. Endoscopic Retrograde Cholangiopancreatography (ERCP) is a crucial procedure for managing a multitude of common pancreaticobiliary conditions. GLP -1 RA use is becoming more prevalent and guidance on the management of GLP-1 RA in the perioperative period is necessary. This is the first study to explore ERCP outcomes in patients using GLP-1 RAs.
Methods: We conducted a retrospective cohort study using large population-based data from the TriNetX platform. We included patients who underwent ERCP and were on GLP-1 RAs between 2018-2024. This cohort of patients was matched with patients who did not receive GLP-1 RAs according to demographics, comorbidities, obesity, BMI, anesthesia medications and confounders that could affect gut motility or aspiration risks using 1:1 propensity score matching (PSM). Primary outcomes included the risk of post-ERCP pancreatitis (PEP), aspiration pneumonia and intubation within 30 days of undergoing ERCP
Results: Before matching, patients who underwent ERCP and were on GLP-1 RAs were at age 60.1 +/- 14.1, white 69.9%, female 54.6%, had higher comorbidities and BMI, table 1. After PSM, we had 3,862 patients in both cohorts. Our study revealed a significantly lower risk of intubation (HR 0.55, 95% CI [0.32-0.93]) and all-cause mortality (HR 0.48, [0.36-0.64]), among patients who underwent ERCP and were on GLP-1 RAs compared to those who were not. There were no statistically significant differences between the two cohorts in the rates of aspiration pneumonia (HR 0.83, [0.53-1.30]) or PEP (HR 0.90, [0.67-1.23]). Figure 1.
Discussion: In our retrospective cohort study, we found that patients on GLP-1RAs were not at a higher risk of developing aspiration pneumonia or requiring emergent intubation compared to patients not on GLP-1RAs. These patients were also not at a higher risk of developing PEP within 30 days of undergoing ERCP. Interestingly, we found that patients on GLP-1RAs had lower rates of all-cause mortality compared to patients not on GLP-1RAs. These findings suggest that the impact of GLP-1RAs might reduce mortality through their anti-inflammatory properties. While these results are promising, further research is necessary to verify the presence of a causal effect and to evaluate the potential benefits of GLP-1RAs in this clinical context.
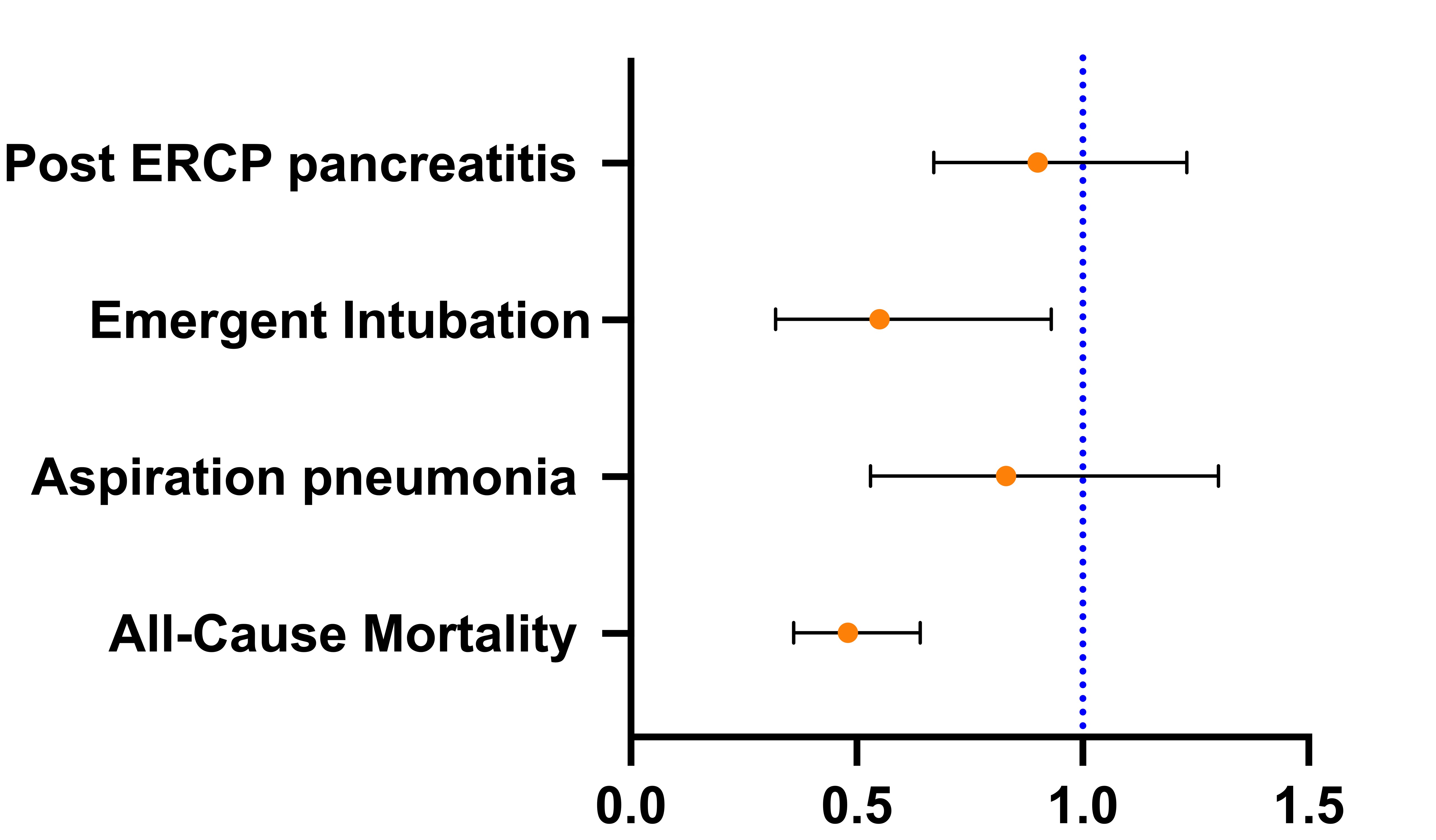
Figure: Figure 1: The risk of Post ERCP pancreatitis, aspiration pneumonia, emergent intubation and All-Cause Mortality within 30 days of undergoing ERCP in GLP-1RAs users vs nonusers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Ahmed El Telbany indicated no relevant financial relationships.
Marina Kim indicated no relevant financial relationships.
Tarek Sawas indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Mahmoud Y. Madi, MD2, Ahmed El Telbany, MD, MPH3, Marina Kim, MD2, Tarek Sawas, MD4. P4471 - Glucagon-Like Peptide-1 Receptor Agonists Are Not Associated With Higher Risk of Intubation or Aspiration Pneumonia in Patients Who Underwent ERCP: A National Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
