Tuesday Poster Session
Category: Interventional Endoscopy
P4495 - Safety and Efficacy of Endoscopic Ultrasound-Guided Pelvic Abscess Drainage: An Updated Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- RL
Ramesh Lamichhane, MBBS
Mayo Clinic School of Graduate Medical Education
Rochester, MN
Presenting Author(s)
Ramesh Lamichhane, MBBS1, Bishnu Deep. Pathak, MBBS2, Ethan M.. Cohen, MD3, Ayowumi A.. Adekolu, MD3, Daniel M. Simadibrata, MD4, Rohit Agrawal, MD5, Shyam Thakkar, MD3
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Nepalese Army Institute of Health Sciences, Kathmandu, Bagmati, Nepal; 3West Virginia University, Morgantown, WV; 4Mayo Clinic, Cleveland, OH; 5West Virginia University School of Medicine, Morgantown, WV
Introduction: Endoscopic ultrasound (EUS)-guided drainage is frequently being used for management of pelvic abscess. It serves as a minimally invasive alternative to surgical or computed tomography (CT)-guided drainage. However, consensus on its efficacy, safety, and adverse events remains limited. Therefore, we aim to provide an updated review of literature evaluating the technical and clinical outcomes including adverse events.
Methods: Literature search was conducted across databases (PubMed, EMBASE, SCOPUS, CINAHL) from inception to May 2024. Inclusion criteria included studies with sample size of more than 5 patients, that reported technical and clinical success, and/or adverse events. The primary outcomes were technical/clinical success, and adverse events. Secondary outcomes included duration of hospital stay and need for repeat intervention. Technical success was defined by successful access to abscess cavity and complete drainage while clinical success was indicated by symptoms remission and resolution of the abscess on follow-up imaging, 1-4 weeks post-procedure.
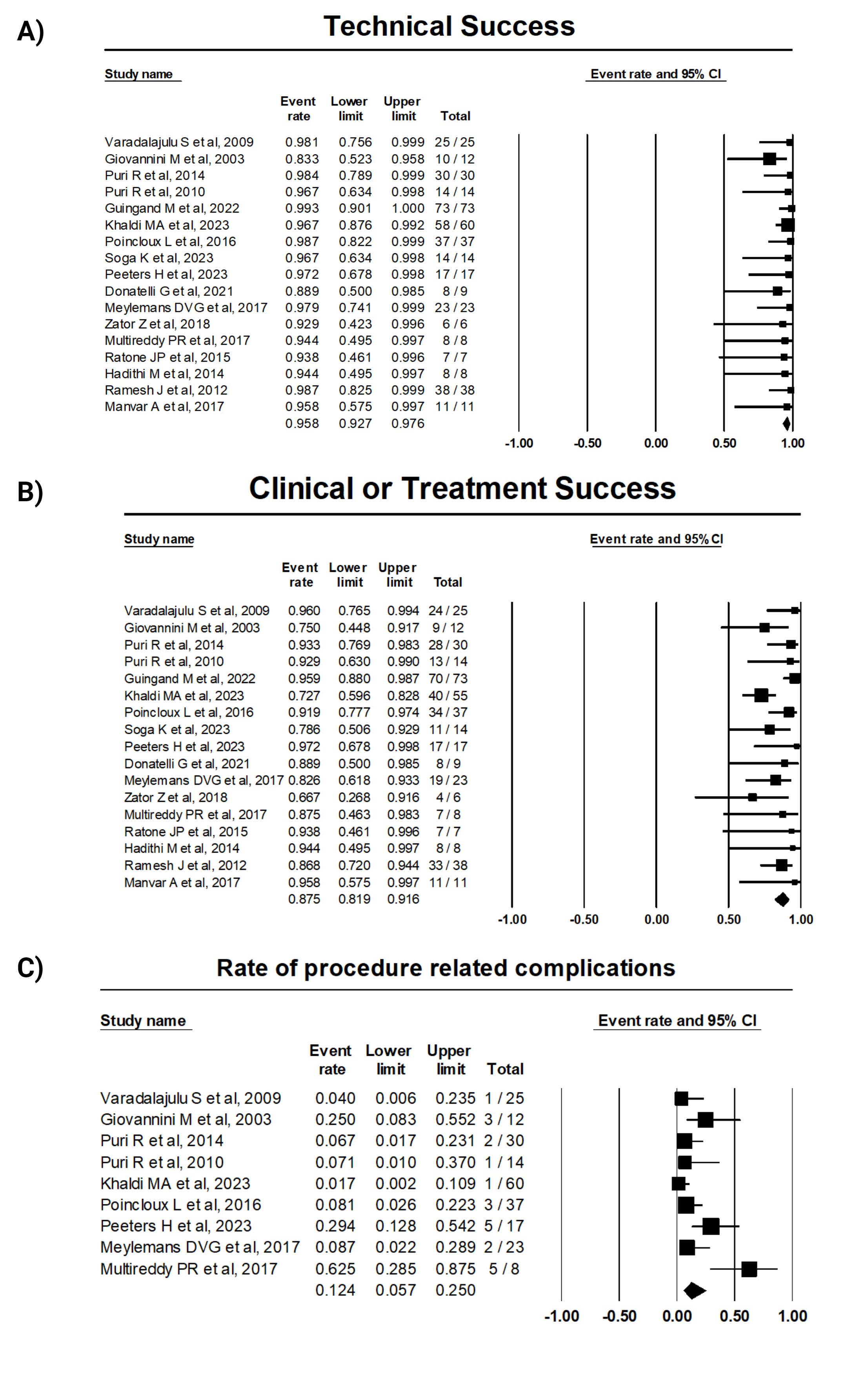
Results: Seventeen studies involving 355 patients undergoing EUS-guided drainage were included. The pooled event rates are as follows: technical success, 95.8% (CI: 0.92 – 0.97; I2: 0); clinical success, 87.5% (CI: 0.82 – 0.92; I2: 33.7%); adverse events 12.4 % (CI: 0.06 – 0.25; I2: 67.4%), recurrence was 7.7% (CI: 0.05 – 0.12; I2: 6.8%), and mean duration of hospital stay was 6±1 days (CI: 4.05 – 8.37; I2: 79.4%) (Figure 1). Stent migration was the most common adverse event (n=13[5.7%]).The subgroup analysis based on the drainage modality showed higher clinical success with the use of stent compared to aspiration only. (Table 1)
Discussion: EUS-guided drainage is an effective and safe approach for managing pelvic abscesses. This updated systematic review and meta-analysis supports the use of EUS-guided drainage as alternative to surgical and CT-guided methods. Future clinical trials are required to validate the differences in success rates between various drainage techniques in patients with pelvic abscesses.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramesh Lamichhane, MBBS1, Bishnu Deep. Pathak, MBBS2, Ethan M.. Cohen, MD3, Ayowumi A.. Adekolu, MD3, Daniel M. Simadibrata, MD4, Rohit Agrawal, MD5, Shyam Thakkar, MD3. P4495 - Safety and Efficacy of Endoscopic Ultrasound-Guided Pelvic Abscess Drainage: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Nepalese Army Institute of Health Sciences, Kathmandu, Bagmati, Nepal; 3West Virginia University, Morgantown, WV; 4Mayo Clinic, Cleveland, OH; 5West Virginia University School of Medicine, Morgantown, WV
Introduction: Endoscopic ultrasound (EUS)-guided drainage is frequently being used for management of pelvic abscess. It serves as a minimally invasive alternative to surgical or computed tomography (CT)-guided drainage. However, consensus on its efficacy, safety, and adverse events remains limited. Therefore, we aim to provide an updated review of literature evaluating the technical and clinical outcomes including adverse events.
Methods: Literature search was conducted across databases (PubMed, EMBASE, SCOPUS, CINAHL) from inception to May 2024. Inclusion criteria included studies with sample size of more than 5 patients, that reported technical and clinical success, and/or adverse events. The primary outcomes were technical/clinical success, and adverse events. Secondary outcomes included duration of hospital stay and need for repeat intervention. Technical success was defined by successful access to abscess cavity and complete drainage while clinical success was indicated by symptoms remission and resolution of the abscess on follow-up imaging, 1-4 weeks post-procedure.
Results: Seventeen studies involving 355 patients undergoing EUS-guided drainage were included. The pooled event rates are as follows: technical success, 95.8% (CI: 0.92 – 0.97; I2: 0); clinical success, 87.5% (CI: 0.82 – 0.92; I2: 33.7%); adverse events 12.4 % (CI: 0.06 – 0.25; I2: 67.4%), recurrence was 7.7% (CI: 0.05 – 0.12; I2: 6.8%), and mean duration of hospital stay was 6±1 days (CI: 4.05 – 8.37; I2: 79.4%) (Figure 1). Stent migration was the most common adverse event (n=13[5.7%]).The subgroup analysis based on the drainage modality showed higher clinical success with the use of stent compared to aspiration only. (Table 1)
Discussion: EUS-guided drainage is an effective and safe approach for managing pelvic abscesses. This updated systematic review and meta-analysis supports the use of EUS-guided drainage as alternative to surgical and CT-guided methods. Future clinical trials are required to validate the differences in success rates between various drainage techniques in patients with pelvic abscesses.
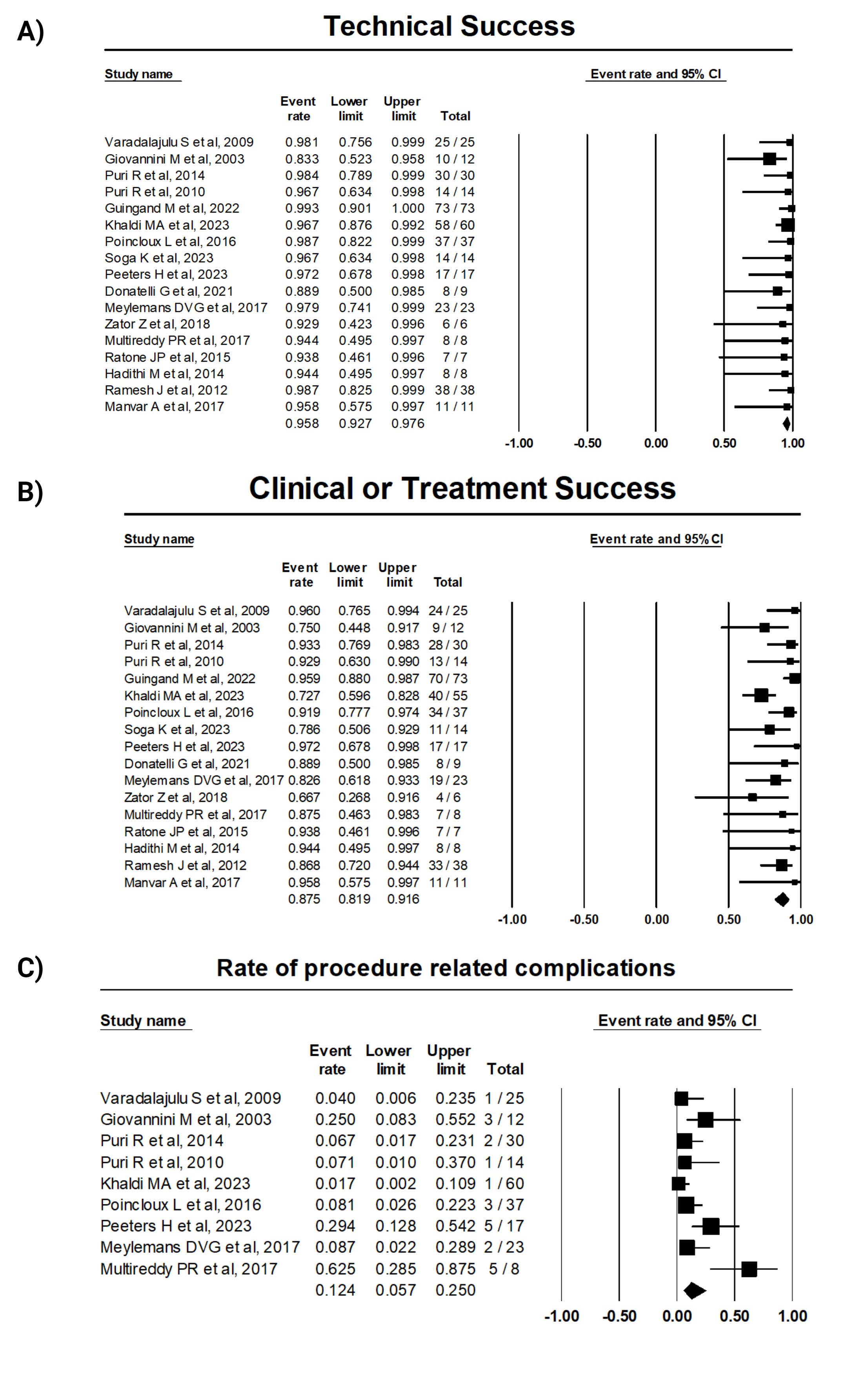
Figure: Figure 1. Outcome of EUS-guided drainage for pelvic abscess. (Panel A-C) Technical success, clinical success, and procedure related complications rate with 95% confidence interval across included studies.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramesh Lamichhane indicated no relevant financial relationships.
Bishnu Pathak indicated no relevant financial relationships.
Ethan Cohen indicated no relevant financial relationships.
Ayowumi Adekolu indicated no relevant financial relationships.
Daniel Simadibrata indicated no relevant financial relationships.
Rohit Agrawal indicated no relevant financial relationships.
Shyam Thakkar: Boston Scientific – Consultant. Guide Point – Consultant. Iterative Scopes – Consultant. Medtronic – Consultant. Steris – Consultant.
Ramesh Lamichhane, MBBS1, Bishnu Deep. Pathak, MBBS2, Ethan M.. Cohen, MD3, Ayowumi A.. Adekolu, MD3, Daniel M. Simadibrata, MD4, Rohit Agrawal, MD5, Shyam Thakkar, MD3. P4495 - Safety and Efficacy of Endoscopic Ultrasound-Guided Pelvic Abscess Drainage: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
