Tuesday Poster Session
Category: Interventional Endoscopy
P4499 - Head-to-Head Comparison of Intragastric Balloon vs Endoscopic Sleeve Gastroplasty for Obesity: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tarek G. Aridi, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Tarek G. Aridi, MD1, Azizullah Beran, MD1, Monzer Abdalla, MD2, Mohammad Al-Haddad, MD, FACG1, Ashley Gilmore, MD3, Mark A. Gromski, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2Ascension Saint Francis Hospital, Evanston, IL; 3Indiana University School of Medicine, Westfield, IN
Introduction: Endoscopic weight loss procedures are gaining popularity due to their minimally invasive nature and positive efficacy profiles. This meta-analysis aims to compare the efficacy of intragastric balloon insertion (IGB) versus endoscopic sleeve gastrectomy (ESG) for the treatment of obesity.
Methods: A comprehensive search of PubMed, Embase, and Web of Science databases was conducted to include all studies directly comparing IGB to ESG. Single-arm studies were excluded. Pooled mean difference (MD) and risk ratio (RR), with 95% confidence intervals (CIs) were obtained within a random-effect model. The primary outcome of interest was the total body weight loss percentage (TBWL%) at 3-months, 6-months, and 12-months. Secondary outcome is the rate of adverse events.
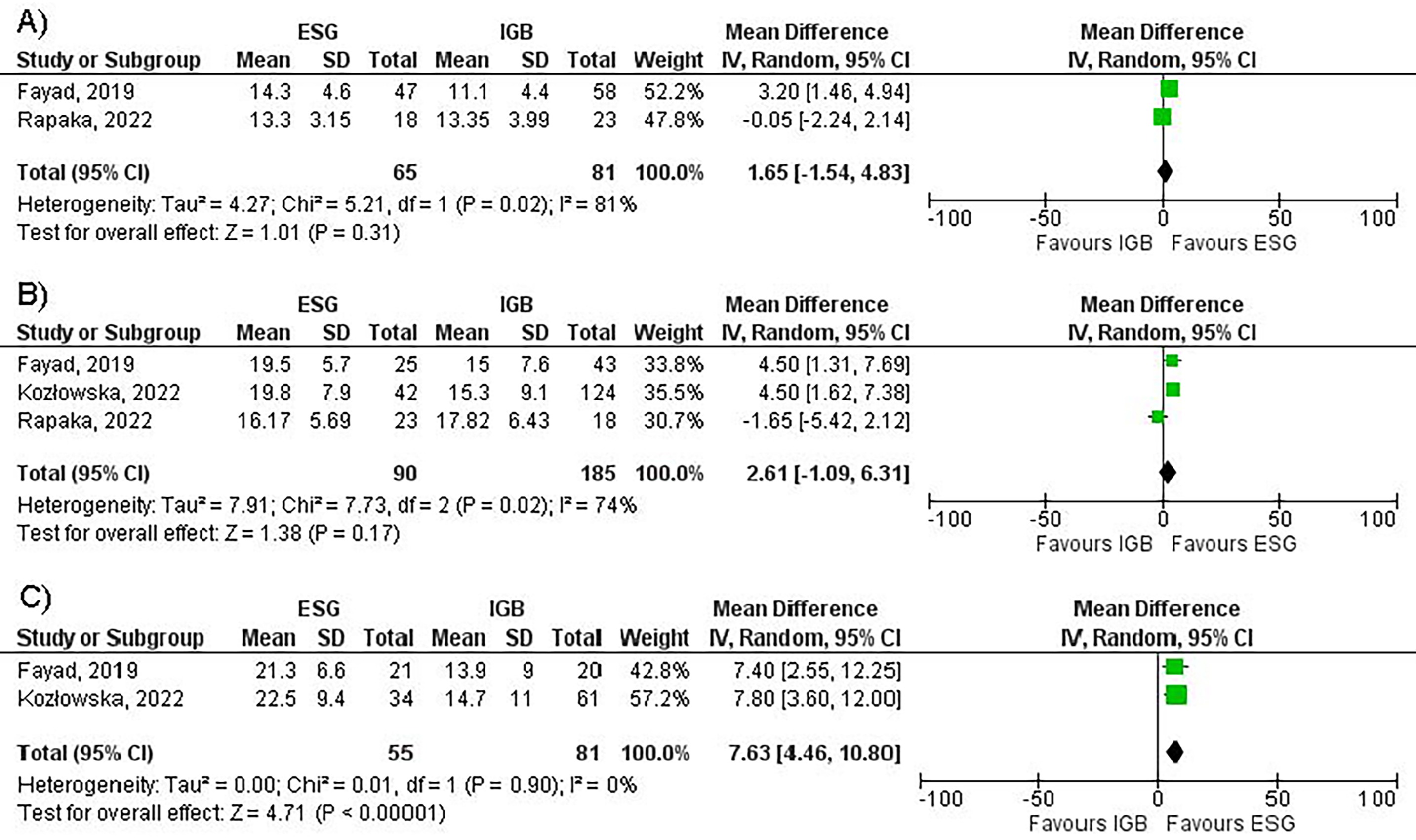
Results: Three studies (two retrospective cohorts and one prospective cohort) with a total of 373 patients with obesity (n= 250 IGB, n= 123 ESG) were included. Females represented 78% of the total patients. The type of IGB was Orbera (Boston Scientific) in all three studies. Mean BMI was 34.9±5.8 and 42.6±6.8 in IGB and ESG groups, respectively. The pooled mean total body weight loss (TBWL) % for IGB at 3, 6, and 12 months were 11.7±4.4, 15.4±8.5 and 14.4±10.1, respectively. The pooled mean TBWL % for ESG at 3, 6, and 12 months were 14±4.2, 19±6.6, and 21.7±7.7, respectively. There was no significant difference between ESG and IGB in TBWL% at 3 months (MD 1.65; 95% CI: -1.54, 4.83; p=0.31; Figure 1A) and 6 months (MD 2.61; 95% CI: -1.09, 6.31; p=0.17, Figure 1B). Compared to IGB, ESG achieved significantly higher TBWL% at 12 months (MD 7.63; 95% CI: 4.46, 10.80; p< 0.001; Figure 1C). A significantly greater rate of adverse events requiring hospitalization or device removal, were reported in the IGB (11.64%) group when compared to the ESG (3%) group (RR 0.43, CI: 0.23, 0.80, p=0.016).
Discussion: Our study demonstrates that both IGB and ESG are effective minimally invasive options for weight loss. However, ESG appears to achieve more durable weight loss with fewer serious adverse events. Nevertheless, IGB might be a suitable option for short-term weight loss in select cohorts of patients.
Disclosures:
Tarek G. Aridi, MD1, Azizullah Beran, MD1, Monzer Abdalla, MD2, Mohammad Al-Haddad, MD, FACG1, Ashley Gilmore, MD3, Mark A. Gromski, MD1. P4499 - Head-to-Head Comparison of Intragastric Balloon vs Endoscopic Sleeve Gastroplasty for Obesity: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Ascension Saint Francis Hospital, Evanston, IL; 3Indiana University School of Medicine, Westfield, IN
Introduction: Endoscopic weight loss procedures are gaining popularity due to their minimally invasive nature and positive efficacy profiles. This meta-analysis aims to compare the efficacy of intragastric balloon insertion (IGB) versus endoscopic sleeve gastrectomy (ESG) for the treatment of obesity.
Methods: A comprehensive search of PubMed, Embase, and Web of Science databases was conducted to include all studies directly comparing IGB to ESG. Single-arm studies were excluded. Pooled mean difference (MD) and risk ratio (RR), with 95% confidence intervals (CIs) were obtained within a random-effect model. The primary outcome of interest was the total body weight loss percentage (TBWL%) at 3-months, 6-months, and 12-months. Secondary outcome is the rate of adverse events.
Results: Three studies (two retrospective cohorts and one prospective cohort) with a total of 373 patients with obesity (n= 250 IGB, n= 123 ESG) were included. Females represented 78% of the total patients. The type of IGB was Orbera (Boston Scientific) in all three studies. Mean BMI was 34.9±5.8 and 42.6±6.8 in IGB and ESG groups, respectively. The pooled mean total body weight loss (TBWL) % for IGB at 3, 6, and 12 months were 11.7±4.4, 15.4±8.5 and 14.4±10.1, respectively. The pooled mean TBWL % for ESG at 3, 6, and 12 months were 14±4.2, 19±6.6, and 21.7±7.7, respectively. There was no significant difference between ESG and IGB in TBWL% at 3 months (MD 1.65; 95% CI: -1.54, 4.83; p=0.31; Figure 1A) and 6 months (MD 2.61; 95% CI: -1.09, 6.31; p=0.17, Figure 1B). Compared to IGB, ESG achieved significantly higher TBWL% at 12 months (MD 7.63; 95% CI: 4.46, 10.80; p< 0.001; Figure 1C). A significantly greater rate of adverse events requiring hospitalization or device removal, were reported in the IGB (11.64%) group when compared to the ESG (3%) group (RR 0.43, CI: 0.23, 0.80, p=0.016).
Discussion: Our study demonstrates that both IGB and ESG are effective minimally invasive options for weight loss. However, ESG appears to achieve more durable weight loss with fewer serious adverse events. Nevertheless, IGB might be a suitable option for short-term weight loss in select cohorts of patients.
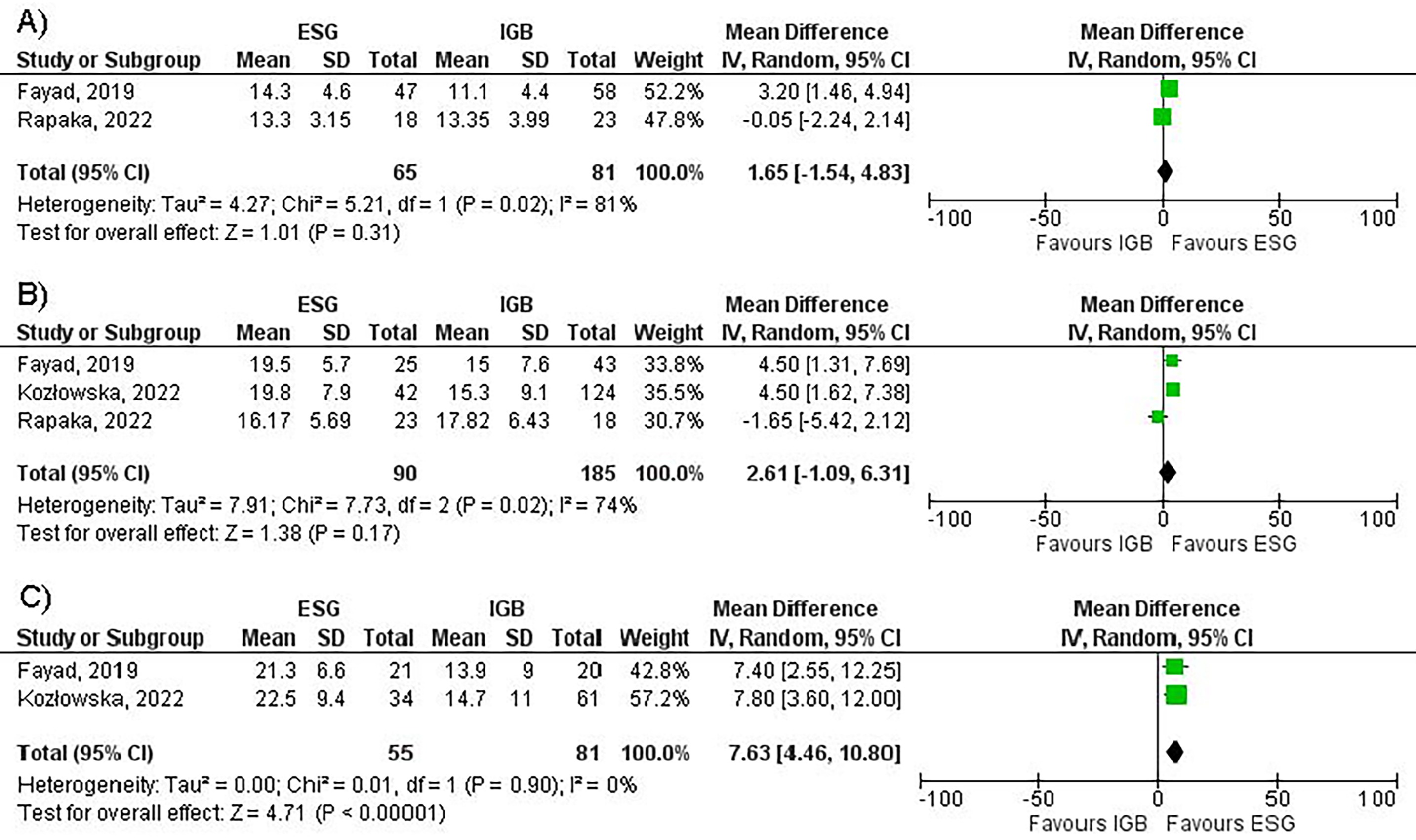
Figure: Figure 1: Forest plots comparing endoscopic sleeve gastroplasty to intragastric balloon for total body weight loss percentage at (A) 3-months, (B) 6-months, and (C) 12-months.
Disclosures:
Tarek Aridi indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
Ashley Gilmore: Allurion – Grant/Research Support.
Mark Gromski: Allurion – Grant/Research Support. Ambu – Consultant. Boston Scientific – Consultant. Cook Medical – Grant/Research Support. Fractyl – Grant/Research Support.
Tarek G. Aridi, MD1, Azizullah Beran, MD1, Monzer Abdalla, MD2, Mohammad Al-Haddad, MD, FACG1, Ashley Gilmore, MD3, Mark A. Gromski, MD1. P4499 - Head-to-Head Comparison of Intragastric Balloon vs Endoscopic Sleeve Gastroplasty for Obesity: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
