Tuesday Poster Session
Category: Interventional Endoscopy
P4527 - Endoscopic Ultrasound-Guided Fine Needle Biopsy Diagnosis of A Rare Retroperitoneal Tumor: Mesenteric Ganglioneuroma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harneet Sangha, BS
Washington State University Elson S. Floyd College of Medicine
Spokane, WA
Presenting Author(s)
Harneet Sangha, BS1, Byung Kim, MD2, Mohamed Alassas, MD2, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Ganglioneuromas (GNs) are rare, accounting for 1% of primary retroperitoneal tumors; they are benign neurogenic tumors typically found in the head/neck, or adrenal glands. Although mostly asymptomatic, large masses may cause symptoms like pain, vomiting, and diarrhea.
Case Description/Methods: A 20-year-old female with no previous illnesses, who vapes once weekly and consumes six alcoholic drinks/week, with a significant family history of breast cancer, presented to the ED after a motor vehicle accident. As part of trauma workup, a computerized tomography (CT) scan incidentally revealed a large vascular mass within the left retroperitoneum, raising concerns about a neoplastic lesion/sarcoma.
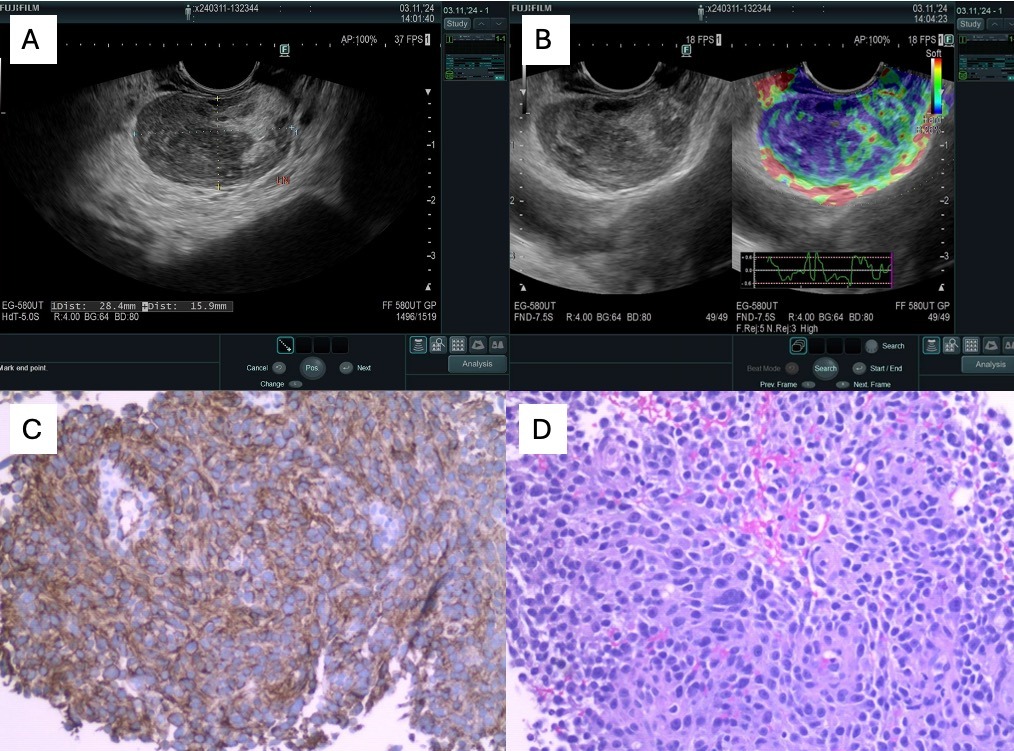
EUS identified a 6x5 cm round heterogeneously hypoechoic retroperitoneal mass, part of which showed inflammatory changes with vascular involvement, bit distinct from pancreas. Pathology from 22-G fine needle biopsy (FNB) revealed a low-grade spindle cell neoplasm composed of wavy nuclei & scattered mature ganglion cells within a collagenous stroma. Immunohistochemical stains showed multifocal positivity for S100, SOX-10 & synaptophysin. The morphologic and immunophenotypic findings were consistent with GN with no evidence of malignancy.
The patient subsequently underwent successful and uneventful surgical removal of the GN.
Discussion: Retroperitoneal Ganglioneuromas (GNs) are rare tumors, arising from sympathetic nervous system (neural crest cells), and are often asymptomatic and hence discovered incidentally, as in our case. The CT imaging for GNs typically lack specific features, and majority of available literature suggests diagnosis on surgical resected specimen.
In our instance, we employed EUS-FNB to identify the GN, to enable appropriate curative surgical planning. Since one of the main differentials was sarcoma, for which a more radical resection with left nephrectomy and potentially left colectomy and distal pancreatectomy was being considered, once diagnosis of benign GN was established with EUS-FNB, a more conservative surgical approach was possible, and saved the patient a more radical surgery.
Complete surgical excision is crucial to prevent recurrence and malignant transformation of GN. Due to their rarity, diagnostic challenges may arise, leading to misdiagnosis or delayed management. In addition, intimacy of the tumor to the retroperitoneal large vessels may limit the surgical resection possibilities, although was successfully accomplished in our case.
Disclosures:
Harneet Sangha, BS1, Byung Kim, MD2, Mohamed Alassas, MD2, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1. P4527 - Endoscopic Ultrasound-Guided Fine Needle Biopsy Diagnosis of A Rare Retroperitoneal Tumor: Mesenteric Ganglioneuroma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Ganglioneuromas (GNs) are rare, accounting for 1% of primary retroperitoneal tumors; they are benign neurogenic tumors typically found in the head/neck, or adrenal glands. Although mostly asymptomatic, large masses may cause symptoms like pain, vomiting, and diarrhea.
Case Description/Methods: A 20-year-old female with no previous illnesses, who vapes once weekly and consumes six alcoholic drinks/week, with a significant family history of breast cancer, presented to the ED after a motor vehicle accident. As part of trauma workup, a computerized tomography (CT) scan incidentally revealed a large vascular mass within the left retroperitoneum, raising concerns about a neoplastic lesion/sarcoma.
EUS identified a 6x5 cm round heterogeneously hypoechoic retroperitoneal mass, part of which showed inflammatory changes with vascular involvement, bit distinct from pancreas. Pathology from 22-G fine needle biopsy (FNB) revealed a low-grade spindle cell neoplasm composed of wavy nuclei & scattered mature ganglion cells within a collagenous stroma. Immunohistochemical stains showed multifocal positivity for S100, SOX-10 & synaptophysin. The morphologic and immunophenotypic findings were consistent with GN with no evidence of malignancy.
The patient subsequently underwent successful and uneventful surgical removal of the GN.
Discussion: Retroperitoneal Ganglioneuromas (GNs) are rare tumors, arising from sympathetic nervous system (neural crest cells), and are often asymptomatic and hence discovered incidentally, as in our case. The CT imaging for GNs typically lack specific features, and majority of available literature suggests diagnosis on surgical resected specimen.
In our instance, we employed EUS-FNB to identify the GN, to enable appropriate curative surgical planning. Since one of the main differentials was sarcoma, for which a more radical resection with left nephrectomy and potentially left colectomy and distal pancreatectomy was being considered, once diagnosis of benign GN was established with EUS-FNB, a more conservative surgical approach was possible, and saved the patient a more radical surgery.
Complete surgical excision is crucial to prevent recurrence and malignant transformation of GN. Due to their rarity, diagnostic challenges may arise, leading to misdiagnosis or delayed management. In addition, intimacy of the tumor to the retroperitoneal large vessels may limit the surgical resection possibilities, although was successfully accomplished in our case.
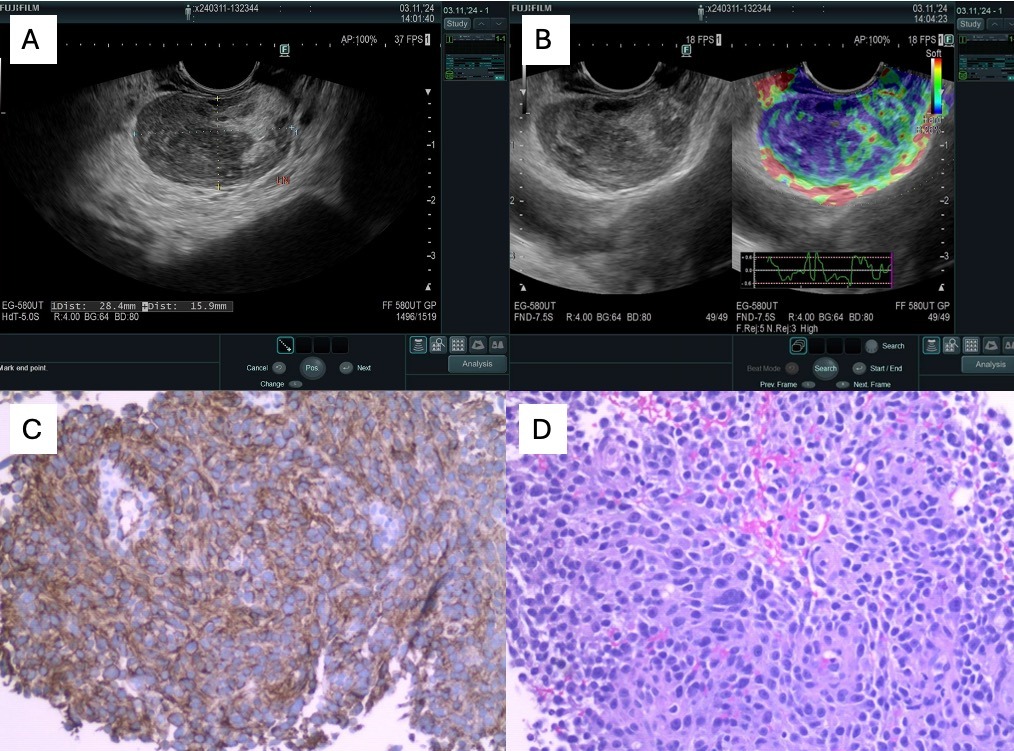
Figure: A: EUS appearance of retroperitoneal heterogeneously hypoechoic mass; B: Successful FNB performed for histology and IHC; C: S100 – Highlighting Schwann cell and ganglion cell components; D: Synaptophysin – highlighting ganglion cells.
Disclosures:
Harneet Sangha indicated no relevant financial relationships.
Byung Kim indicated no relevant financial relationships.
Mohamed Alassas indicated no relevant financial relationships.
Tavishi Girotra indicated no relevant financial relationships.
Shreya Chopra indicated no relevant financial relationships.
Navansh Johnson indicated no relevant financial relationships.
Anusha Singhania indicated no relevant financial relationships.
Mohit Girotra indicated no relevant financial relationships.
Harneet Sangha, BS1, Byung Kim, MD2, Mohamed Alassas, MD2, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1. P4527 - Endoscopic Ultrasound-Guided Fine Needle Biopsy Diagnosis of A Rare Retroperitoneal Tumor: Mesenteric Ganglioneuroma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
