Tuesday Poster Session
Category: Interventional Endoscopy
P4551 - Unique Approach to Managing Hepatojejunal Anastomosis Stricture in a Patient with Long Roux-en-Y Limb
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Paxton Smith, MD
Providence Sacred Heart Medical Center
Cheney, WA
Presenting Author(s)
Award: Presidential Poster Award
Paxton Smith, MD1, Nishant Puri, MD, FACG2
1Providence Sacred Heart Medical Center, Cheney, WA; 2Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Stricture of hepaticojejunostomy (HJ) is a common adverse outcome in patients who undergo Roux-en-Y hepaticojejunostomy after injury of the common bile duct during cholecystectomy. Strictures in this area are typically managed with an Enteroscopy assisted Endoscopic Retrograde Cholangiopancreatography (ERCP) or endoscopic ultrasound (EUS) guided hepatico-gastrostomy (HG). We report a patient in whom a device assisted ERCP could not be completed and describe a novel approach to HJ stricture management.
Case Description/Methods: A 52-year-old woman with a history of iatrogenic injury during cholecystectomy 28 years ago, managed with Roux-en-Y hepaticojejunostomy underwent a right hepatectomy for ongoing biliary stricture 8 years later. Later, she developed an abscess in the right liver resection site managed with percutaneous drains. Subsequent imaging showed a HJ stricture. Patient underwent an attempt at device assisted ERCP, but the HJ could not be reached due to long Roux limb. She then underwent EUS guided HG with placement of a fully covered metal stent and a double pigtail stent into the left intrahepatic duct for biliary decompression. She developed choledocholithiasis above the HJ stricture and then presented to our facility for replacement of stents and clearance of stones. However, endoscopic exam demonstrated HG stents positioned just past the GE junction creating difficult access for repeated procedures. Therefore, a novel approach was utilized. After identifying the HJ, an EUS guided duodenojejunostomy was created close to the HJ using a cautery enhanced lumen opposing metal stent. This enabled standard duodenoscope access to the HJ and performance of ERCP, dilation and resolution of the HJ stricture and clearance of the choledocholithiasis. The previously placed hepatico-gastrostomy stents were terminally removed. The patient had normalization of liver associated enzymes and was asymptomatic at 6-month follow-up without need for further endoscopic or radiological studies.
Discussion: EUS-guided biliary access is occasionally used to facilitate bile drainage in select patients with altered foregut anatomy. In this patient, a HG facilitated biliary drainage of bile, but required multiple endoscopic interventions without resolution of the underlying HJ stricture. Our novel approach of EUS-guided duodenojejunostomy enabled durable long-term access to the HJ stricture, resolution of the underlying HJ stricture and definitive therapy for choledocholithiasis.
Disclosures:
Paxton Smith, MD1, Nishant Puri, MD, FACG2. P4551 - Unique Approach to Managing Hepatojejunal Anastomosis Stricture in a Patient with Long Roux-en-Y Limb, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Paxton Smith, MD1, Nishant Puri, MD, FACG2
1Providence Sacred Heart Medical Center, Cheney, WA; 2Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Stricture of hepaticojejunostomy (HJ) is a common adverse outcome in patients who undergo Roux-en-Y hepaticojejunostomy after injury of the common bile duct during cholecystectomy. Strictures in this area are typically managed with an Enteroscopy assisted Endoscopic Retrograde Cholangiopancreatography (ERCP) or endoscopic ultrasound (EUS) guided hepatico-gastrostomy (HG). We report a patient in whom a device assisted ERCP could not be completed and describe a novel approach to HJ stricture management.
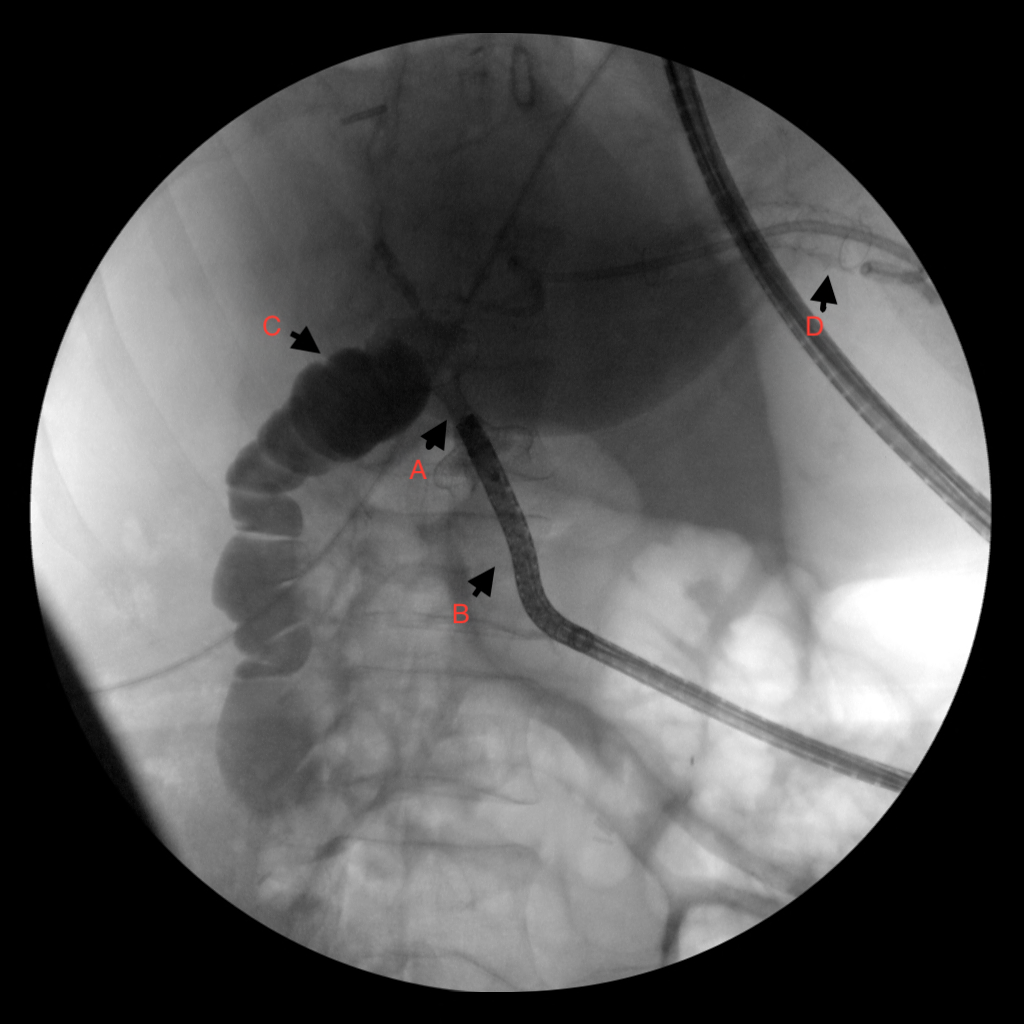
Case Description/Methods: A 52-year-old woman with a history of iatrogenic injury during cholecystectomy 28 years ago, managed with Roux-en-Y hepaticojejunostomy underwent a right hepatectomy for ongoing biliary stricture 8 years later. Later, she developed an abscess in the right liver resection site managed with percutaneous drains. Subsequent imaging showed a HJ stricture. Patient underwent an attempt at device assisted ERCP, but the HJ could not be reached due to long Roux limb. She then underwent EUS guided HG with placement of a fully covered metal stent and a double pigtail stent into the left intrahepatic duct for biliary decompression. She developed choledocholithiasis above the HJ stricture and then presented to our facility for replacement of stents and clearance of stones. However, endoscopic exam demonstrated HG stents positioned just past the GE junction creating difficult access for repeated procedures. Therefore, a novel approach was utilized. After identifying the HJ, an EUS guided duodenojejunostomy was created close to the HJ using a cautery enhanced lumen opposing metal stent. This enabled standard duodenoscope access to the HJ and performance of ERCP, dilation and resolution of the HJ stricture and clearance of the choledocholithiasis. The previously placed hepatico-gastrostomy stents were terminally removed. The patient had normalization of liver associated enzymes and was asymptomatic at 6-month follow-up without need for further endoscopic or radiological studies.
Discussion: EUS-guided biliary access is occasionally used to facilitate bile drainage in select patients with altered foregut anatomy. In this patient, a HG facilitated biliary drainage of bile, but required multiple endoscopic interventions without resolution of the underlying HJ stricture. Our novel approach of EUS-guided duodenojejunostomy enabled durable long-term access to the HJ stricture, resolution of the underlying HJ stricture and definitive therapy for choledocholithiasis.
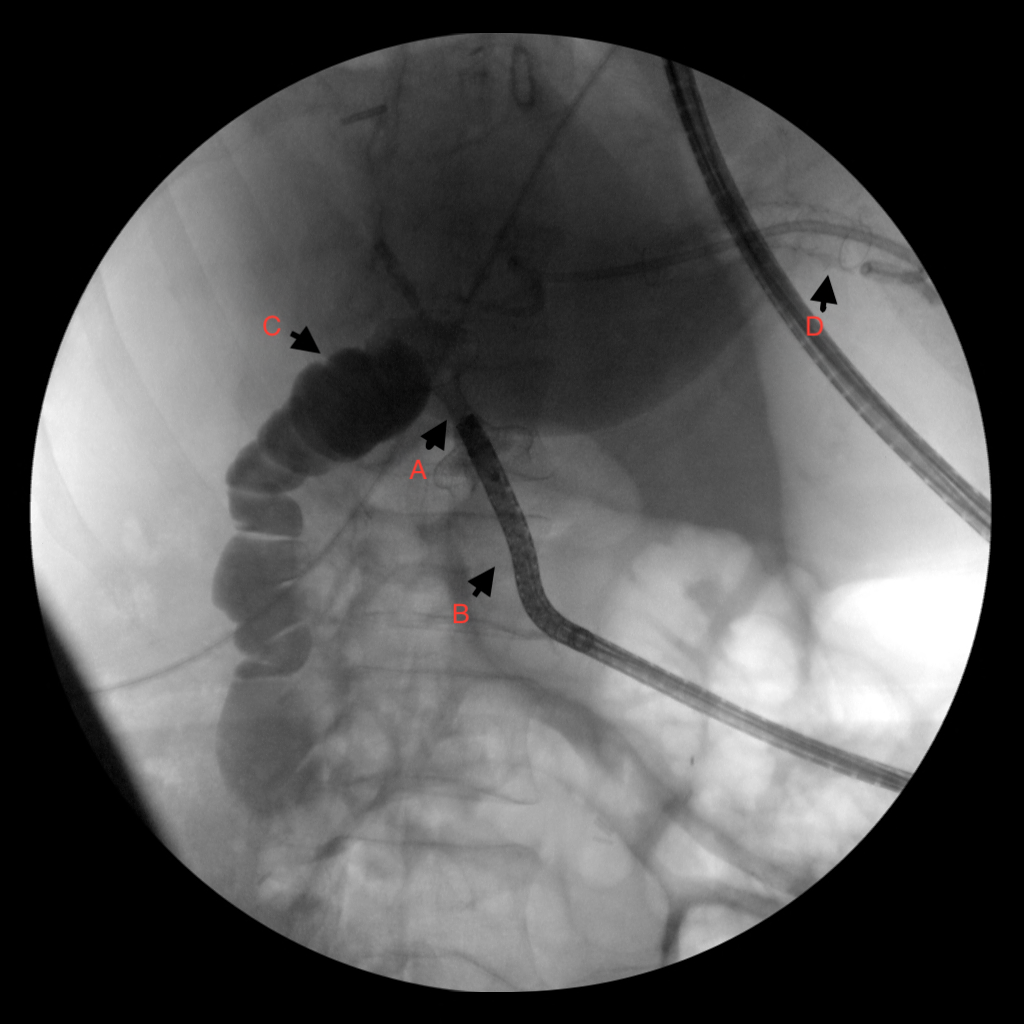
Figure: Image demonstrating placement of duodenojejunostomy with flow of contrast agent.
A: Axios stent, B: Duodenum, C: Biliary Limb, D: Hepaticogastrostomy
A: Axios stent, B: Duodenum, C: Biliary Limb, D: Hepaticogastrostomy
Disclosures:
Paxton Smith indicated no relevant financial relationships.
Nishant Puri: Boston Scientific – Consultant.
Paxton Smith, MD1, Nishant Puri, MD, FACG2. P4551 - Unique Approach to Managing Hepatojejunal Anastomosis Stricture in a Patient with Long Roux-en-Y Limb, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


