Tuesday Poster Session
Category: Interventional Endoscopy
P4555 - Beyond the Norm: Intraductal Papillary Mucinous Neoplasm With an Unusual Presentation Mimicking Gastric Outlet Obstruction – A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Pearl Aggarwal, MD
University Hospitals St. John Medical Center
Westlake, OH
Presenting Author(s)
Pearl Aggarwal, MD1, Saqr Alsakarneh, MD2, Farah A. Khraisat, MD3, Fatema Dinary, 4, Soukaina El Yazal, MD5, Fazel Dinary, MD1
1University Hospitals St. John Medical Center, Westlake, OH; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 4Case Western Reserve University, Cleveland, OH; 5Ministry of Health, Zagora, Souss-Massa-Dr, Morocco
Introduction: Intraductal papillary mucinous neoplasms (IPMN) are cystic neoplasms of the pancreas that develop within the main pancreatic duct or its branches. IPMN presentations range from asymptomatic incidental findings to symptoms similar to pancreatitis due to mucin obstruction.
We report a case of a large side branch IPMN mimicking gastric outlet obstruction, underscoring the need for a multidisciplinary approach in diagnosis and management due to the potential risk of malignancy.
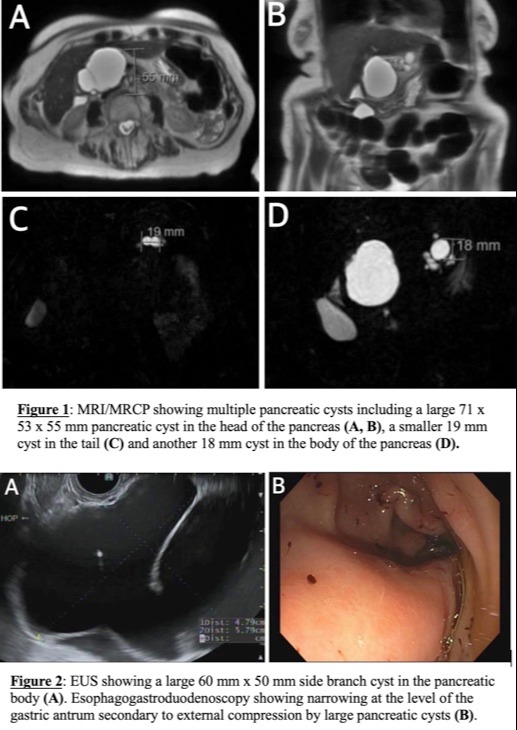
Case Description/Methods: An 87-year-old woman with a history of hypertension presented with worsening abdominal pain, nausea, vomiting, and weight loss over two months. Laboratory studies showed bilirubin at 1.4 mg/dL, lipase at 206 U/L, and Carcinoma 19-9 at 12.06 U/L, with normal liver function tests. MRI/MRCP indicated mild gastric distention suggestive of gastric outlet obstruction and identified a large side branch IPMN (71 mm x 53 mm x 55 mm) in the head, a 19 mm cyst in the tail, and an 18 mm cyst in the body of the pancreas (Figure 1). Endoscopic ultrasonography (EUS) revealed anechoic cystic and multiple thinly septate lesions in the pancreatic head (55 mm x 35 mm), body (60 mm x 50 mm) (Figure 2-A), and tail (20 mm x 15 mm), with no solid internal debris. The main pancreatic duct was dilated up to 3 mm. Esophagogastroduodenoscopy showed narrowing at the gastric antrum due to external compression by the cysts (Figure 2-B). EUS-guided drainage was performed, aspirating 200 ml of viscous, clear fluid using a 19-gauge FNA needle. The string test was positive. Cytology and fluid analysis revealed glucose < 10 mg/dL, amylase < 10 U/L, and CEA at 851.8 µg/L. Symptoms gradually resolved, and the patient was scheduled for a repeat MRI/MRCP after one year.
Discussion: This is the first reported case of a large IPMN presenting as gastric outlet obstruction. It highlights an unusual presentation of IPMN, stressing the importance of considering IPMNs in cases of dyspepsia and weight loss. The case also emphasizes the role of EUS-guided aspiration in diagnosis and symptom relief. The presence of multiple cysts and their large size (≥30 mm) raises concerns about malignant potential. Effective management of IPMNs requires evaluating factors such as duct involvement, lesion size, mural nodules, and duct dilation, underscoring the need for early endoscopic intervention in suspected cases.
Disclosures:
Pearl Aggarwal, MD1, Saqr Alsakarneh, MD2, Farah A. Khraisat, MD3, Fatema Dinary, 4, Soukaina El Yazal, MD5, Fazel Dinary, MD1. P4555 - Beyond the Norm: Intraductal Papillary Mucinous Neoplasm With an Unusual Presentation Mimicking Gastric Outlet Obstruction – A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals St. John Medical Center, Westlake, OH; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 4Case Western Reserve University, Cleveland, OH; 5Ministry of Health, Zagora, Souss-Massa-Dr, Morocco
Introduction: Intraductal papillary mucinous neoplasms (IPMN) are cystic neoplasms of the pancreas that develop within the main pancreatic duct or its branches. IPMN presentations range from asymptomatic incidental findings to symptoms similar to pancreatitis due to mucin obstruction.
We report a case of a large side branch IPMN mimicking gastric outlet obstruction, underscoring the need for a multidisciplinary approach in diagnosis and management due to the potential risk of malignancy.
Case Description/Methods: An 87-year-old woman with a history of hypertension presented with worsening abdominal pain, nausea, vomiting, and weight loss over two months. Laboratory studies showed bilirubin at 1.4 mg/dL, lipase at 206 U/L, and Carcinoma 19-9 at 12.06 U/L, with normal liver function tests. MRI/MRCP indicated mild gastric distention suggestive of gastric outlet obstruction and identified a large side branch IPMN (71 mm x 53 mm x 55 mm) in the head, a 19 mm cyst in the tail, and an 18 mm cyst in the body of the pancreas (Figure 1). Endoscopic ultrasonography (EUS) revealed anechoic cystic and multiple thinly septate lesions in the pancreatic head (55 mm x 35 mm), body (60 mm x 50 mm) (Figure 2-A), and tail (20 mm x 15 mm), with no solid internal debris. The main pancreatic duct was dilated up to 3 mm. Esophagogastroduodenoscopy showed narrowing at the gastric antrum due to external compression by the cysts (Figure 2-B). EUS-guided drainage was performed, aspirating 200 ml of viscous, clear fluid using a 19-gauge FNA needle. The string test was positive. Cytology and fluid analysis revealed glucose < 10 mg/dL, amylase < 10 U/L, and CEA at 851.8 µg/L. Symptoms gradually resolved, and the patient was scheduled for a repeat MRI/MRCP after one year.
Discussion: This is the first reported case of a large IPMN presenting as gastric outlet obstruction. It highlights an unusual presentation of IPMN, stressing the importance of considering IPMNs in cases of dyspepsia and weight loss. The case also emphasizes the role of EUS-guided aspiration in diagnosis and symptom relief. The presence of multiple cysts and their large size (≥30 mm) raises concerns about malignant potential. Effective management of IPMNs requires evaluating factors such as duct involvement, lesion size, mural nodules, and duct dilation, underscoring the need for early endoscopic intervention in suspected cases.
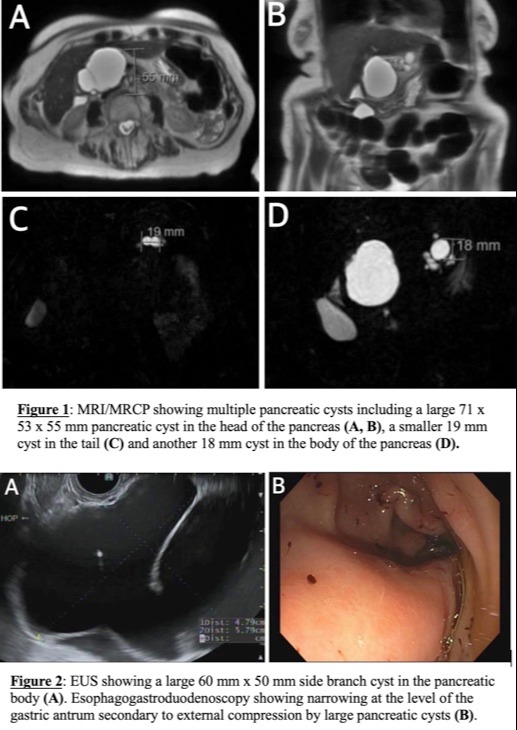
Figure: Figures
Disclosures:
Pearl Aggarwal indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Farah A. Khraisat indicated no relevant financial relationships.
Fatema Dinary indicated no relevant financial relationships.
Soukaina El Yazal indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Pearl Aggarwal, MD1, Saqr Alsakarneh, MD2, Farah A. Khraisat, MD3, Fatema Dinary, 4, Soukaina El Yazal, MD5, Fazel Dinary, MD1. P4555 - Beyond the Norm: Intraductal Papillary Mucinous Neoplasm With an Unusual Presentation Mimicking Gastric Outlet Obstruction – A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
