Tuesday Poster Session
Category: Interventional Endoscopy
P4564 - Navigating Unresectable Pancreatic Masses: An Endoscopic Ultrasound-Guided Approach to Biliary Drainage in a Patient With an Indwelling Luminal Stent
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rama Hussein, DO
Mount Sinai Morningside/West
New York, NY
Presenting Author(s)
Rama Hussein, DO1, Marni H. Wilkoff, DO1, Neal Shah, DO2, Rashmi Advani, MD3
1Mount Sinai Morningside/West, New York, NY; 2Mount Sinai South Nassau, New York, NY; 3Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Pancreatic cancer causes symptomatic gastric outlet obstruction (GOO) in about 15-20% of patients. Endoscopic luminal stenting is preferred over palliative surgery as it provides immediate relief, decreases morbidity and improves 30-day quality of life, however tumor invasion (26%) and biliary obstruction (59%) are common complications. As pancreatic tumors progress, they can lead to biliary obstruction, more commonly than GOO. Endoscopic ultrasound-guided choledochoduedenostomy (EUS-CDS) is a noninvasive approach used to relieve biliary obstruction in cases with difficult biliary cannulation. Luminal access through the duodenal bulb must be preserved to employ this approach. This case outlines a patient with a pancreatic head mass that initially was treated with an uncovered luminal stent for duodenal obstruction who later required endoscopic treatment of biliary obstruction.
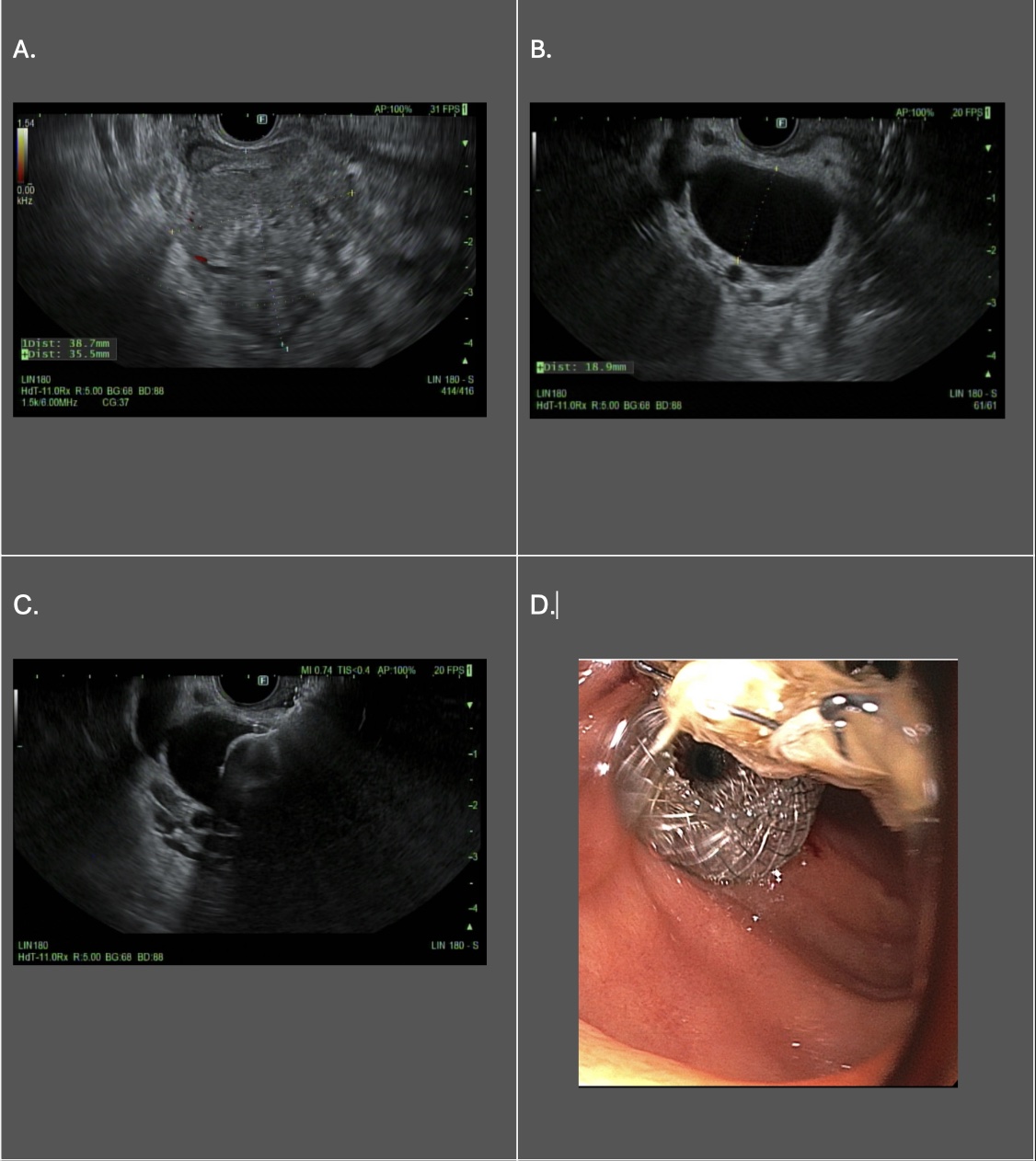
Case Description/Methods: An 89-year-old male with hypertension and diabetes was admitted for nausea and vomiting. Liver tests were normal and CT imaging showed a significantly distended stomach secondary to a 4.3 cm pancreatic mass, resulting in duodenal obstruction. EUS-guided core biopsies confirmed moderately-differentiated pancreatic adenocarcinoma. An uncovered luminal stent was placed to treat the GOO. An overall non-surgical approach was ensued given the non-operable extent of disease. Months later, he presented with obstructive jaundice. ERCP revealed complete tissue ingrowth at major papilla precluding conventional retrograde access to the biliary tree. Despite an indwelling luminal stent, a safe endosonographic window was found from the duodenal bulb to the distended bile duct and an EUS-CDS was successfully placed resulting in biliary decompression. His liver enzymes significantly improved and was discharged to home hospice.
Discussion: EUS-guided therapies including EUS-CDS are non-invasive, non-surgical, quality-of-life preserving techniques in patients with difficult retrograde biliary access. It is crucial to understand that biliary obstruction may eventually present with GOO in pancreatic head cancers. Appropriate therapies which would not only reduce complications associated with luminal stents but would allow for future EUS-guided access to the bile duct through the duodenum need to be considered. EUS-guided gastrojejunostomy is one approach and may be pursued if local expertise is available. An alternate approach is also prophylactic biliary stenting, if feasible, for patients presenting with GOO.
Disclosures:
Rama Hussein, DO1, Marni H. Wilkoff, DO1, Neal Shah, DO2, Rashmi Advani, MD3. P4564 - Navigating Unresectable Pancreatic Masses: An Endoscopic Ultrasound-Guided Approach to Biliary Drainage in a Patient With an Indwelling Luminal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Morningside/West, New York, NY; 2Mount Sinai South Nassau, New York, NY; 3Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Pancreatic cancer causes symptomatic gastric outlet obstruction (GOO) in about 15-20% of patients. Endoscopic luminal stenting is preferred over palliative surgery as it provides immediate relief, decreases morbidity and improves 30-day quality of life, however tumor invasion (26%) and biliary obstruction (59%) are common complications. As pancreatic tumors progress, they can lead to biliary obstruction, more commonly than GOO. Endoscopic ultrasound-guided choledochoduedenostomy (EUS-CDS) is a noninvasive approach used to relieve biliary obstruction in cases with difficult biliary cannulation. Luminal access through the duodenal bulb must be preserved to employ this approach. This case outlines a patient with a pancreatic head mass that initially was treated with an uncovered luminal stent for duodenal obstruction who later required endoscopic treatment of biliary obstruction.
Case Description/Methods: An 89-year-old male with hypertension and diabetes was admitted for nausea and vomiting. Liver tests were normal and CT imaging showed a significantly distended stomach secondary to a 4.3 cm pancreatic mass, resulting in duodenal obstruction. EUS-guided core biopsies confirmed moderately-differentiated pancreatic adenocarcinoma. An uncovered luminal stent was placed to treat the GOO. An overall non-surgical approach was ensued given the non-operable extent of disease. Months later, he presented with obstructive jaundice. ERCP revealed complete tissue ingrowth at major papilla precluding conventional retrograde access to the biliary tree. Despite an indwelling luminal stent, a safe endosonographic window was found from the duodenal bulb to the distended bile duct and an EUS-CDS was successfully placed resulting in biliary decompression. His liver enzymes significantly improved and was discharged to home hospice.
Discussion: EUS-guided therapies including EUS-CDS are non-invasive, non-surgical, quality-of-life preserving techniques in patients with difficult retrograde biliary access. It is crucial to understand that biliary obstruction may eventually present with GOO in pancreatic head cancers. Appropriate therapies which would not only reduce complications associated with luminal stents but would allow for future EUS-guided access to the bile duct through the duodenum need to be considered. EUS-guided gastrojejunostomy is one approach and may be pursued if local expertise is available. An alternate approach is also prophylactic biliary stenting, if feasible, for patients presenting with GOO.
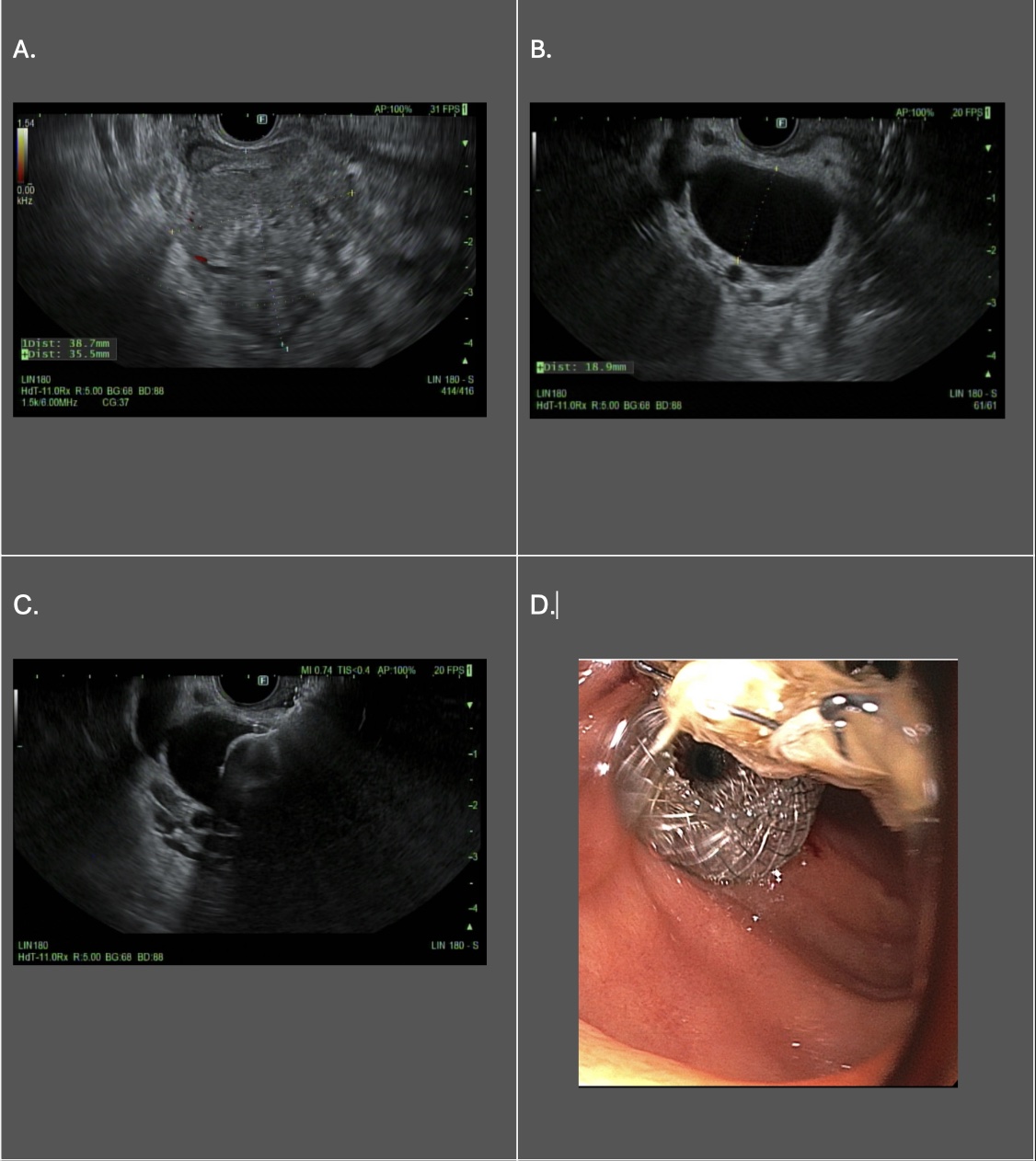
Figure: Figure 1. Initial Endoscopic ultrasound revealing initial pancreatic head mass (A.) Repeat EUS revealing dilated CBD (B), the deployment of luminal stent into CBD (C) and post EUS-CDS (D).
Disclosures:
Rama Hussein indicated no relevant financial relationships.
Marni Wilkoff indicated no relevant financial relationships.
Neal Shah indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Rama Hussein, DO1, Marni H. Wilkoff, DO1, Neal Shah, DO2, Rashmi Advani, MD3. P4564 - Navigating Unresectable Pancreatic Masses: An Endoscopic Ultrasound-Guided Approach to Biliary Drainage in a Patient With an Indwelling Luminal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
