Tuesday Poster Session
Category: Liver
P4593 - Herpes Zoster Infection in Cirrhosis Patients: A National Inpatient Database Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad U. Kamal, MD
Hackensack Meridian Health
Roselle Park, NJ
Presenting Author(s)
Muhammad Kamal, MD1, Umar Hayat, MD2, Fnu Faheela, MBBS3, Sandesh Parajuli, MD4, Aamir Saeed, MD5, Hasan Zerti, MD2, Shiva Naidoo, MD2, Manesh Kumar Gangwani, MD6, Umer Farooq, MD7, Fnu Vikash, MD, M.Med8, Amna Iqbal, MD9, Faisal Kamal, MD10, Zubair Khan, MD11
1Hackensack Meridian Health, Roselle Park, NJ; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Reading Hospital - Tower Health, Reading, PA; 5Vanderbilt University Medical Center, Nashville, TN; 6University of Toledo, Toledo, OH; 7SSM Health Saint Louis University Hospital, St. Louis, MO; 8Albert Einstein College of Medicine, New York, NY; 9University of Toledo Medical Center, Toledo, OH; 10Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 11Mercy Hospital Jefferson, Festus, MO
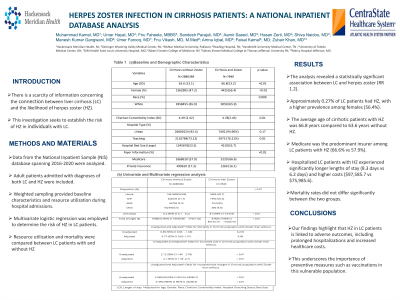
Introduction: There is a scarcity of information concerning the connection between liver cirrhosis (LC) and the likelihood of herpes zoster (HZ). This investigation seeks to establish the risk of HZ in individuals with LC.
Methods: Data from the National Inpatient Sample (NIS) database spanning 2016-2020 were analyzed. Adult patients admitted with diagnoses of both LC and HZ were included. Weighted sampling provided baseline characteristics and resource utilization during hospital admissions. Multivariate logistic regression was employed to determine the risk of HZ in LC patients. Resource utilization and mortality were compared between LC patients with and without HZ.
Results: The analysis revealed a statistically significant association between LC and herpes zoster (RR 1.2). Approximately 0.27% of LC patients had HZ, with a higher prevalence among females (56.4%). The average age of cirrhotic patients with HZ was 66.8 years compared to 63.6 years without HZ. Those with HZ had a higher Charlson Comorbidity Index (CCI) score (4.78 vs 4.49). Medicare was the predominant insurer among LC patients with HZ (66.6% vs 57.9%). Hospitalized LC patients with HZ experienced significantly longer lengths of stay (8.3 days vs 6.2 days) and higher costs ($97,585.7 vs $75,985.6). Mortality rates did not differ significantly between the two groups.
Discussion: Our findings highlight that HZ in LC patients is linked to adverse outcomes, including prolonged hospitalizations and increased healthcare costs. This underscores the importance of preventive measures such as vaccinations in this vulnerable population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Kamal, MD1, Umar Hayat, MD2, Fnu Faheela, MBBS3, Sandesh Parajuli, MD4, Aamir Saeed, MD5, Hasan Zerti, MD2, Shiva Naidoo, MD2, Manesh Kumar Gangwani, MD6, Umer Farooq, MD7, Fnu Vikash, MD, M.Med8, Amna Iqbal, MD9, Faisal Kamal, MD10, Zubair Khan, MD11. P4593 - Herpes Zoster Infection in Cirrhosis Patients: A National Inpatient Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Hackensack Meridian Health, Roselle Park, NJ; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3Nishtar Medical University, Multan, Punjab, Pakistan; 4Reading Hospital - Tower Health, Reading, PA; 5Vanderbilt University Medical Center, Nashville, TN; 6University of Toledo, Toledo, OH; 7SSM Health Saint Louis University Hospital, St. Louis, MO; 8Albert Einstein College of Medicine, New York, NY; 9University of Toledo Medical Center, Toledo, OH; 10Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 11Mercy Hospital Jefferson, Festus, MO
Introduction: There is a scarcity of information concerning the connection between liver cirrhosis (LC) and the likelihood of herpes zoster (HZ). This investigation seeks to establish the risk of HZ in individuals with LC.
Methods: Data from the National Inpatient Sample (NIS) database spanning 2016-2020 were analyzed. Adult patients admitted with diagnoses of both LC and HZ were included. Weighted sampling provided baseline characteristics and resource utilization during hospital admissions. Multivariate logistic regression was employed to determine the risk of HZ in LC patients. Resource utilization and mortality were compared between LC patients with and without HZ.
Results: The analysis revealed a statistically significant association between LC and herpes zoster (RR 1.2). Approximately 0.27% of LC patients had HZ, with a higher prevalence among females (56.4%). The average age of cirrhotic patients with HZ was 66.8 years compared to 63.6 years without HZ. Those with HZ had a higher Charlson Comorbidity Index (CCI) score (4.78 vs 4.49). Medicare was the predominant insurer among LC patients with HZ (66.6% vs 57.9%). Hospitalized LC patients with HZ experienced significantly longer lengths of stay (8.3 days vs 6.2 days) and higher costs ($97,585.7 vs $75,985.6). Mortality rates did not differ significantly between the two groups.
Discussion: Our findings highlight that HZ in LC patients is linked to adverse outcomes, including prolonged hospitalizations and increased healthcare costs. This underscores the importance of preventive measures such as vaccinations in this vulnerable population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Kamal indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Fnu Faheela indicated no relevant financial relationships.
Sandesh Parajuli indicated no relevant financial relationships.
Aamir Saeed indicated no relevant financial relationships.
Hasan Zerti indicated no relevant financial relationships.
Shiva Naidoo indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Amna Iqbal indicated no relevant financial relationships.
Faisal Kamal indicated no relevant financial relationships.
Zubair Khan indicated no relevant financial relationships.
Muhammad Kamal, MD1, Umar Hayat, MD2, Fnu Faheela, MBBS3, Sandesh Parajuli, MD4, Aamir Saeed, MD5, Hasan Zerti, MD2, Shiva Naidoo, MD2, Manesh Kumar Gangwani, MD6, Umer Farooq, MD7, Fnu Vikash, MD, M.Med8, Amna Iqbal, MD9, Faisal Kamal, MD10, Zubair Khan, MD11. P4593 - Herpes Zoster Infection in Cirrhosis Patients: A National Inpatient Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
