Tuesday Poster Session
Category: Liver
P4597 - Optimizing Discharge Efficiency for Patients With Liver Disease: Harnessing Stressors, and Building Ownership for Lasting Improvement
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JC
John Cooper, MD
University of Alabama at Birmingham Heersink School of Medicine
Birmingham, AL
Presenting Author(s)
John Cooper, MD1, Anyet Belyeu, NP2, Carletta Dobbins, 2, Reid Eagleson, MS2, Allyson Hall, PhD2, Frederick Van Pelt, MD, MBA2, Sujan Ravi, MD, MPH1
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Large healthcare systems often struggle with inefficiencies in the discharge process leading to higher costs, extended hospital stays, and boarding in the emergency department. These challenges could be more pronounced in patients with complex medical conditions such as decompensated cirrhosis and those who receive post-liver transplant care. We describe our approach to tackling discharge delays for patients on the inpatient hepatology service at a large academic liver transplant center.
Methods: The hepatology accountable care team (ACT) is a comprehensive group including attending physicians, trainees, nurses, therapists, pharmacists, care coordinators, and administrative support staff. With the facilitation of the Clinical Practice Transformation (CPT) team, the ACT employed the 3D Problem SolvingTM (3DPSTM) framework to improve its efficiency. During the first phase of 3DPS– “Discovery”- the ACT identified 70 issues which were then categorized into 7 themes in the second phase – “Distill”. The third phase- “Define”- is guided by the Pareto principle that 80% of system challenges could be alleviated by solving 20% of the highest-impact issues. For the Hepatology ACT “Optimizing Team Communication to Coordinate Transitions of Care (ToC)” emerged as the focus area. Through analysis of current state, ToC rounds were identified as the critical 20%. A gap analysis informed the restructuring of ToC rounds with clear roles, responsibilities and a standardized script. In addition, a streamlined onboarding process for trainees was also created with user-friendly videos and printed materials to ensure understanding of the discharge process.
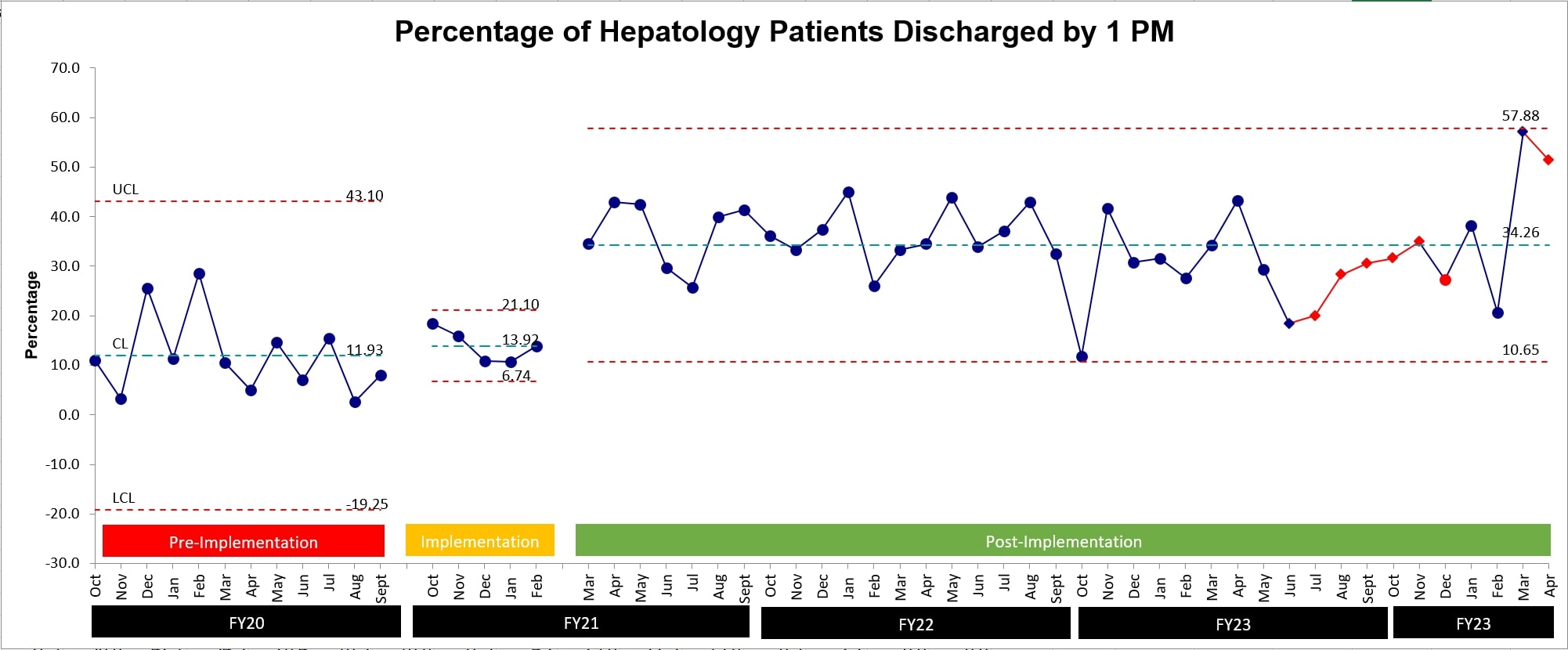
Results: Efficiency of the discharge process was measured as the percentage of discharges completed by 1 PM. Before the employment of 3DPSTM methodology and instituting changes to ToC rounds and resident onboarding, the average discharge efficiency was at 11.93%. Since the implementation of these initiatives, this figure significantly increased to 34.26%, demonstrating a 187% change. This improvement showed consistent progress and peaked at 57.88%.
Discussion: The 3DPSTM utilizes a systems-based strategy allowing care teams to select and address specific relevant problems thereby increasing engagement. This framework enabled the hepatology ACT to identify uncoordinated care transition planning and trainee onboarding as critical factors. Addressing these challenges has enabled significant improvement in discharge efficiency and maintained them consistently.
Disclosures:
John Cooper, MD1, Anyet Belyeu, NP2, Carletta Dobbins, 2, Reid Eagleson, MS2, Allyson Hall, PhD2, Frederick Van Pelt, MD, MBA2, Sujan Ravi, MD, MPH1. P4597 - Optimizing Discharge Efficiency for Patients With Liver Disease: Harnessing Stressors, and Building Ownership for Lasting Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL
Introduction: Large healthcare systems often struggle with inefficiencies in the discharge process leading to higher costs, extended hospital stays, and boarding in the emergency department. These challenges could be more pronounced in patients with complex medical conditions such as decompensated cirrhosis and those who receive post-liver transplant care. We describe our approach to tackling discharge delays for patients on the inpatient hepatology service at a large academic liver transplant center.
Methods: The hepatology accountable care team (ACT) is a comprehensive group including attending physicians, trainees, nurses, therapists, pharmacists, care coordinators, and administrative support staff. With the facilitation of the Clinical Practice Transformation (CPT) team, the ACT employed the 3D Problem SolvingTM (3DPSTM) framework to improve its efficiency. During the first phase of 3DPS– “Discovery”- the ACT identified 70 issues which were then categorized into 7 themes in the second phase – “Distill”. The third phase- “Define”- is guided by the Pareto principle that 80% of system challenges could be alleviated by solving 20% of the highest-impact issues. For the Hepatology ACT “Optimizing Team Communication to Coordinate Transitions of Care (ToC)” emerged as the focus area. Through analysis of current state, ToC rounds were identified as the critical 20%. A gap analysis informed the restructuring of ToC rounds with clear roles, responsibilities and a standardized script. In addition, a streamlined onboarding process for trainees was also created with user-friendly videos and printed materials to ensure understanding of the discharge process.
Results: Efficiency of the discharge process was measured as the percentage of discharges completed by 1 PM. Before the employment of 3DPSTM methodology and instituting changes to ToC rounds and resident onboarding, the average discharge efficiency was at 11.93%. Since the implementation of these initiatives, this figure significantly increased to 34.26%, demonstrating a 187% change. This improvement showed consistent progress and peaked at 57.88%.
Discussion: The 3DPSTM utilizes a systems-based strategy allowing care teams to select and address specific relevant problems thereby increasing engagement. This framework enabled the hepatology ACT to identify uncoordinated care transition planning and trainee onboarding as critical factors. Addressing these challenges has enabled significant improvement in discharge efficiency and maintained them consistently.
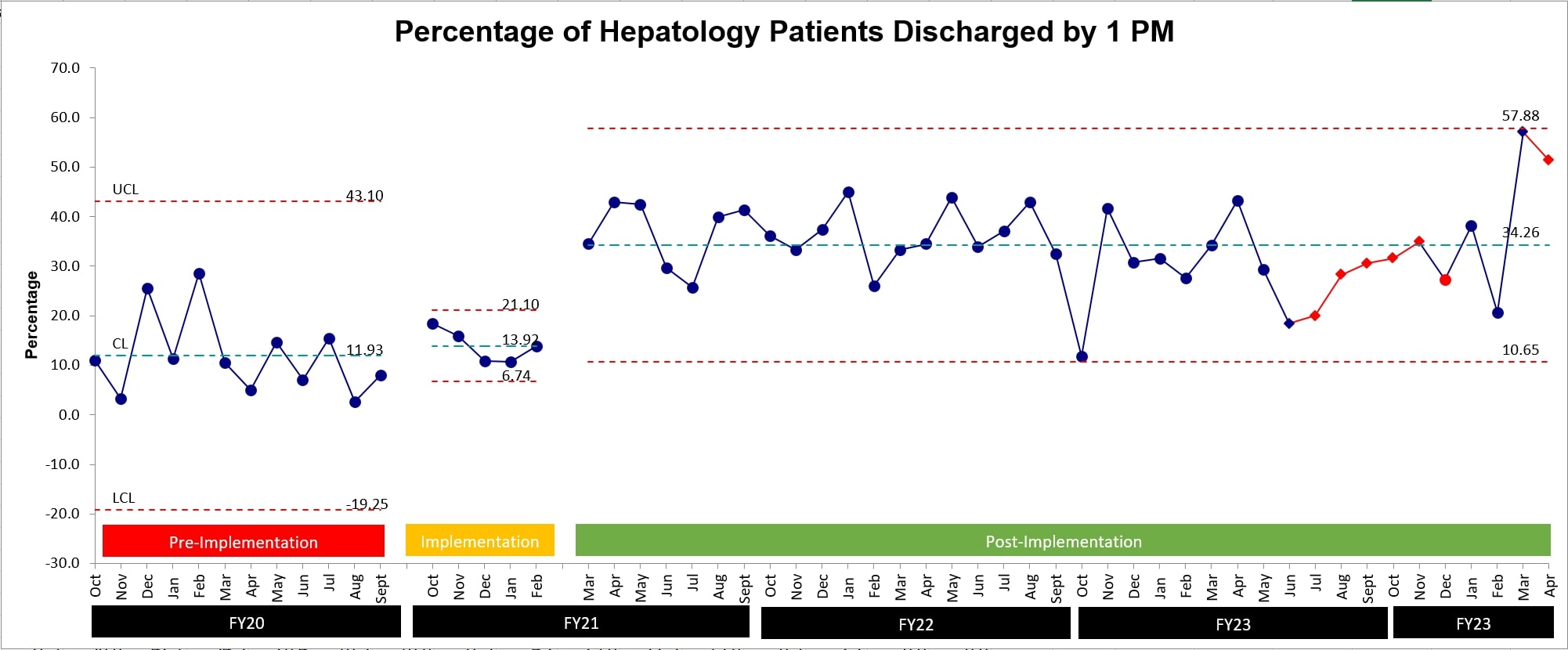
Figure: Percent of Hepatology Patients Discharged by 1 PM
Disclosures:
John Cooper indicated no relevant financial relationships.
Anyet Belyeu indicated no relevant financial relationships.
Carletta Dobbins indicated no relevant financial relationships.
Reid Eagleson indicated no relevant financial relationships.
Allyson Hall indicated no relevant financial relationships.
Frederick Van Pelt indicated no relevant financial relationships.
Sujan Ravi indicated no relevant financial relationships.
John Cooper, MD1, Anyet Belyeu, NP2, Carletta Dobbins, 2, Reid Eagleson, MS2, Allyson Hall, PhD2, Frederick Van Pelt, MD, MBA2, Sujan Ravi, MD, MPH1. P4597 - Optimizing Discharge Efficiency for Patients With Liver Disease: Harnessing Stressors, and Building Ownership for Lasting Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
