Tuesday Poster Session
Category: Liver
P4603 - A Systematic Review of Percutaneous Endoscopic Gastrostomy Placement in Patients with Cirrhosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Umme Jannatul Ferdaush, MD
Tidal Health
Lewes, DE
Presenting Author(s)
Umme Jannatul Ferdaush, MD1, Benjamin Twery, MD2, Justin Canakis, DO3, Dushyant S. Dahiya, MD4, Patricia Ludwig, 5, Jerrold Canakis, MD1, Andrew Canakis, DO6
1Tidal Health, Salisbury, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 4The University of Kansas School of Medicine, Kansas City, KS; 5Richard A. Henson Research Institute, Tidal Health Peninsula Regional, Salisbury, MD; 6University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
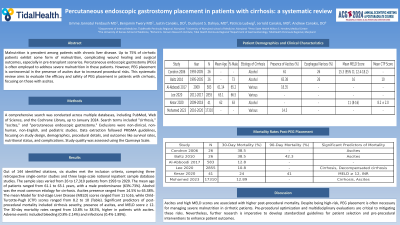
Introduction: Malnutrition is prevalent among patients with chronic liver disease. Up to 75% of cirrhotic patients exhibit some form of malnutrition, complicating wound healing and surgical outcomes, especially in pre-transplant scenarios. Percutaneous endoscopic gastrostomy (PEG) is often employed to address severe malnutrition in these patients. However, PEG placement is controversial in the presence of ascites due to increased procedural risks. This systematic review aims to evaluate the efficacy and safety of PEG placement in patients with cirrhosis, focusing on those with ascites.
Methods: A comprehensive search was conducted across multiple databases, including PubMed, Web of Science, and the Cochrane Library, up to January 2024. Search terms included "cirrhosis," "ascites," and "percutaneous endoscopic gastrostomy." Exclusions were non-clinical, non-human, non-English, and pediatric studies. Data extraction followed PRISMA guidelines, focusing on study design, demographics, procedural details, and outcomes like survival rates, nutritional status, and complications. Study quality was assessed using the Qumseya Scale.
Results: Out of 144 identified citations, six studies met the inclusion criteria, comprising three retrospective single-center studies and three large-scale national inpatient sample database studies. The sample sizes varied from 26 to 17,310 patients from 1993 to 2020. The mean age of patients ranged from 61.1 to 63.1 years, with a male predominance (63%-73%). Alcohol was the most common etiology for cirrhosis. Ascites presence ranged from 14.5% to 65.38%. The mean Model for End-stage Liver Disease (MELD) scores ranged from 11 to 16, while Child-Turcotte-Pugh (CTP) scores ranged from 8.2 to 10 (Table). Significant predictors of post-procedural mortality included cirrhosis severity, presence of ascites, and MELD score ≥ 12. The 30-day mortality rates ranged from 10.8% to 38.5%, higher in patients with ascites. Adverse events included bleeding (0.8%-2.14%) and infections (0.4%-1.89%).
Discussion: Ascites and high MELD scores are associated with higher post-procedural mortality. Despite being high-risk, PEG placement is often necessary for managing severe malnutrition in cirrhotic patients. Pre-procedural optimization and multidisciplinary evaluations are critical to mitigating these risks. Nevertheless, further research is imperative to develop standardized guidelines for patient selection and pre-procedural interventions to enhance patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Umme Jannatul Ferdaush, MD1, Benjamin Twery, MD2, Justin Canakis, DO3, Dushyant S. Dahiya, MD4, Patricia Ludwig, 5, Jerrold Canakis, MD1, Andrew Canakis, DO6. P4603 - A Systematic Review of Percutaneous Endoscopic Gastrostomy Placement in Patients with Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tidal Health, Salisbury, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 4The University of Kansas School of Medicine, Kansas City, KS; 5Richard A. Henson Research Institute, Tidal Health Peninsula Regional, Salisbury, MD; 6University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
Introduction: Malnutrition is prevalent among patients with chronic liver disease. Up to 75% of cirrhotic patients exhibit some form of malnutrition, complicating wound healing and surgical outcomes, especially in pre-transplant scenarios. Percutaneous endoscopic gastrostomy (PEG) is often employed to address severe malnutrition in these patients. However, PEG placement is controversial in the presence of ascites due to increased procedural risks. This systematic review aims to evaluate the efficacy and safety of PEG placement in patients with cirrhosis, focusing on those with ascites.
Methods: A comprehensive search was conducted across multiple databases, including PubMed, Web of Science, and the Cochrane Library, up to January 2024. Search terms included "cirrhosis," "ascites," and "percutaneous endoscopic gastrostomy." Exclusions were non-clinical, non-human, non-English, and pediatric studies. Data extraction followed PRISMA guidelines, focusing on study design, demographics, procedural details, and outcomes like survival rates, nutritional status, and complications. Study quality was assessed using the Qumseya Scale.
Results: Out of 144 identified citations, six studies met the inclusion criteria, comprising three retrospective single-center studies and three large-scale national inpatient sample database studies. The sample sizes varied from 26 to 17,310 patients from 1993 to 2020. The mean age of patients ranged from 61.1 to 63.1 years, with a male predominance (63%-73%). Alcohol was the most common etiology for cirrhosis. Ascites presence ranged from 14.5% to 65.38%. The mean Model for End-stage Liver Disease (MELD) scores ranged from 11 to 16, while Child-Turcotte-Pugh (CTP) scores ranged from 8.2 to 10 (Table). Significant predictors of post-procedural mortality included cirrhosis severity, presence of ascites, and MELD score ≥ 12. The 30-day mortality rates ranged from 10.8% to 38.5%, higher in patients with ascites. Adverse events included bleeding (0.8%-2.14%) and infections (0.4%-1.89%).
Discussion: Ascites and high MELD scores are associated with higher post-procedural mortality. Despite being high-risk, PEG placement is often necessary for managing severe malnutrition in cirrhotic patients. Pre-procedural optimization and multidisciplinary evaluations are critical to mitigating these risks. Nevertheless, further research is imperative to develop standardized guidelines for patient selection and pre-procedural interventions to enhance patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Umme Jannatul Ferdaush indicated no relevant financial relationships.
Benjamin Twery indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Patricia Ludwig indicated no relevant financial relationships.
Jerrold Canakis indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Umme Jannatul Ferdaush, MD1, Benjamin Twery, MD2, Justin Canakis, DO3, Dushyant S. Dahiya, MD4, Patricia Ludwig, 5, Jerrold Canakis, MD1, Andrew Canakis, DO6. P4603 - A Systematic Review of Percutaneous Endoscopic Gastrostomy Placement in Patients with Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
