Tuesday Poster Session
Category: Liver
P4606 - Increasing Provider Comfort With Initiating Advance Care Planning Discussions and Medical Power of Attorney Documentation for Patients With Cirrhosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Priyanka Jagannathan, MD
University of Texas at Austin Dell Medical School
Austin, TX
Presenting Author(s)
Priyanka Jagannathan, MD, Victoria Cooremans, MD, Veronica Chavez, MD, Lillianne Villarreal, MD, Cristal Brown, MD, MHS, Brandon Altillo, MD, MPH
University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Patients with end-stage liver disease (ESLD) have high morbidity and mortality but extremely low rates of advance care planning conversations, including documentation of medical power of attorney (MPOA). Up to 80% of patients with ESLD may develop hepatic encephalopathy during the trajectory of disease, negatively affecting their decision-making capacity1. Initiating advanced care planning (ACP) conversations early in the disease course is essential to preserving patient autonomy surrounding health decisions.
This project aims to improve resident comfort in initiating ACP conversations and MPOA documentation for patients with ESLD.
Methods: Internal medicine (IM) residents at a local federally-qualified health center (FQHC) completed a baseline survey assessing knowledge and comfort of initiating ACP conversations. They subsequently received a 45-minute virtual lecture from a palliative care fellow on initiating ACP and MPOA documentation.
Patients with cirrhosis without MPOA documentation with scheduled appointments within 90 days were identified through chart review. IM residents providing primary care to these patients were contacted via the electronic health record to recommend discussion of MPOA. A post-intervention survey was distributed at the end of the 6-month intervention window.
Results: Pre-intervention survey was completed by 18 residents of which 77.8% of residents did not know a MPOA could be completed in clinic. Average self-reported comfort with completing a MPOA was 2.8 (Scale: 1 not at all comfortable to 5 extremely comfortable). Post-study survey results (n=12) indicated 100% of surveyed residents knew that a MPOA can be completed in clinic (X2 (1, N = 30)= 17.5, p < .001), and average rated comfort with this process 3.6, (t(28)= 2.0, p = .048).
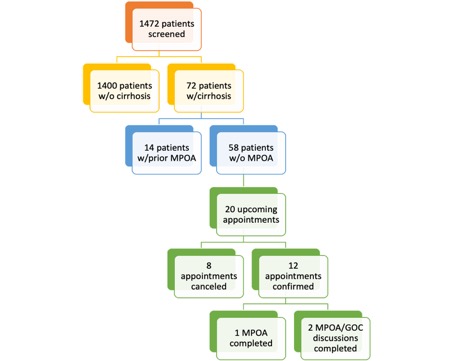
The first study cycle included 12 patient encounters, out of which 1 MPOA was completed and 2 MPOA discussions were documented (Figure 1).
Discussion: There is an overwhelming need for early initiation of ACP in the outpatient setting for patients with ESLD.2 Our project resulted in an improvement in addressing MPOA in patient encounters and a statistically significant increase in self-reported comfort on initiating ACP discussions. Limitations of this study include small sample size, no-show rate, and limited continuity of care. Future directions include qualitative interviews to elucidate barriers to ACP discussions in residency primary care clinic and implementation of workflows tailored to these barriers.
Disclosures:
Priyanka Jagannathan, MD, Victoria Cooremans, MD, Veronica Chavez, MD, Lillianne Villarreal, MD, Cristal Brown, MD, MHS, Brandon Altillo, MD, MPH. P4606 - Increasing Provider Comfort With Initiating Advance Care Planning Discussions and Medical Power of Attorney Documentation for Patients With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Patients with end-stage liver disease (ESLD) have high morbidity and mortality but extremely low rates of advance care planning conversations, including documentation of medical power of attorney (MPOA). Up to 80% of patients with ESLD may develop hepatic encephalopathy during the trajectory of disease, negatively affecting their decision-making capacity1. Initiating advanced care planning (ACP) conversations early in the disease course is essential to preserving patient autonomy surrounding health decisions.
This project aims to improve resident comfort in initiating ACP conversations and MPOA documentation for patients with ESLD.
Methods: Internal medicine (IM) residents at a local federally-qualified health center (FQHC) completed a baseline survey assessing knowledge and comfort of initiating ACP conversations. They subsequently received a 45-minute virtual lecture from a palliative care fellow on initiating ACP and MPOA documentation.
Patients with cirrhosis without MPOA documentation with scheduled appointments within 90 days were identified through chart review. IM residents providing primary care to these patients were contacted via the electronic health record to recommend discussion of MPOA. A post-intervention survey was distributed at the end of the 6-month intervention window.
Results: Pre-intervention survey was completed by 18 residents of which 77.8% of residents did not know a MPOA could be completed in clinic. Average self-reported comfort with completing a MPOA was 2.8 (Scale: 1 not at all comfortable to 5 extremely comfortable). Post-study survey results (n=12) indicated 100% of surveyed residents knew that a MPOA can be completed in clinic (X2 (1, N = 30)= 17.5, p < .001), and average rated comfort with this process 3.6, (t(28)= 2.0, p = .048).
The first study cycle included 12 patient encounters, out of which 1 MPOA was completed and 2 MPOA discussions were documented (Figure 1).
Discussion: There is an overwhelming need for early initiation of ACP in the outpatient setting for patients with ESLD.2 Our project resulted in an improvement in addressing MPOA in patient encounters and a statistically significant increase in self-reported comfort on initiating ACP discussions. Limitations of this study include small sample size, no-show rate, and limited continuity of care. Future directions include qualitative interviews to elucidate barriers to ACP discussions in residency primary care clinic and implementation of workflows tailored to these barriers.
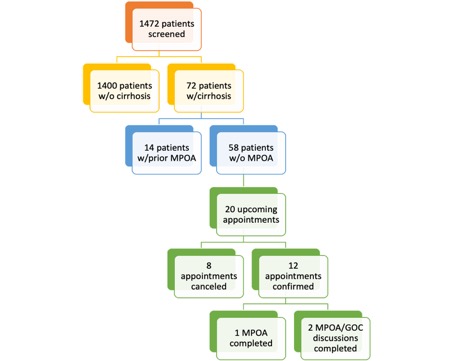
Figure: Flow diagram depicting patient screening for eligibility to undergo intervention (ie, MPOA discussion and/or documentation).
Legend:
Medical Power of Attorney (MPOA)
Goals of Care (GOC)
Legend:
Medical Power of Attorney (MPOA)
Goals of Care (GOC)
Disclosures:
Priyanka Jagannathan indicated no relevant financial relationships.
Victoria Cooremans indicated no relevant financial relationships.
Veronica Chavez indicated no relevant financial relationships.
Lillianne Villarreal indicated no relevant financial relationships.
Cristal Brown indicated no relevant financial relationships.
Brandon Altillo indicated no relevant financial relationships.
Priyanka Jagannathan, MD, Victoria Cooremans, MD, Veronica Chavez, MD, Lillianne Villarreal, MD, Cristal Brown, MD, MHS, Brandon Altillo, MD, MPH. P4606 - Increasing Provider Comfort With Initiating Advance Care Planning Discussions and Medical Power of Attorney Documentation for Patients With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
