Tuesday Poster Session
Category: Liver
P4614 - Assessing the Role of Donated Medications in Post-Liver Transplant Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YW
Yael Wollstein, MD
University of Chicago Medicine
Chicago, IL
Presenting Author(s)
Yael Wollstein, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD
University of Chicago Medicine, Chicago, IL
Introduction: Significant financial toxicity is associated with chronic liver disease (CLD) and post-liver transplant (LT) care due to complex care needs including extensive medication regimens. This can pose a barrier to LT and even those with health insurance can suffer life-threatening gaps in coverage, with a patchwork of systems in place to mitigate the situation. However, given LT medication regimens are often dynamic based on a patient’s clinical situation, prescribed medications can go unused and be discarded. Illinois (IL) state law allows unopened and unexpired medications to be donated and reused. Donated medications have been used to fill gaps in insurance in other states and could be useful for patients with CLD. The aim of this study was to characterize the quantity and type of unused LT medications and determine whether they could be used for other patients.
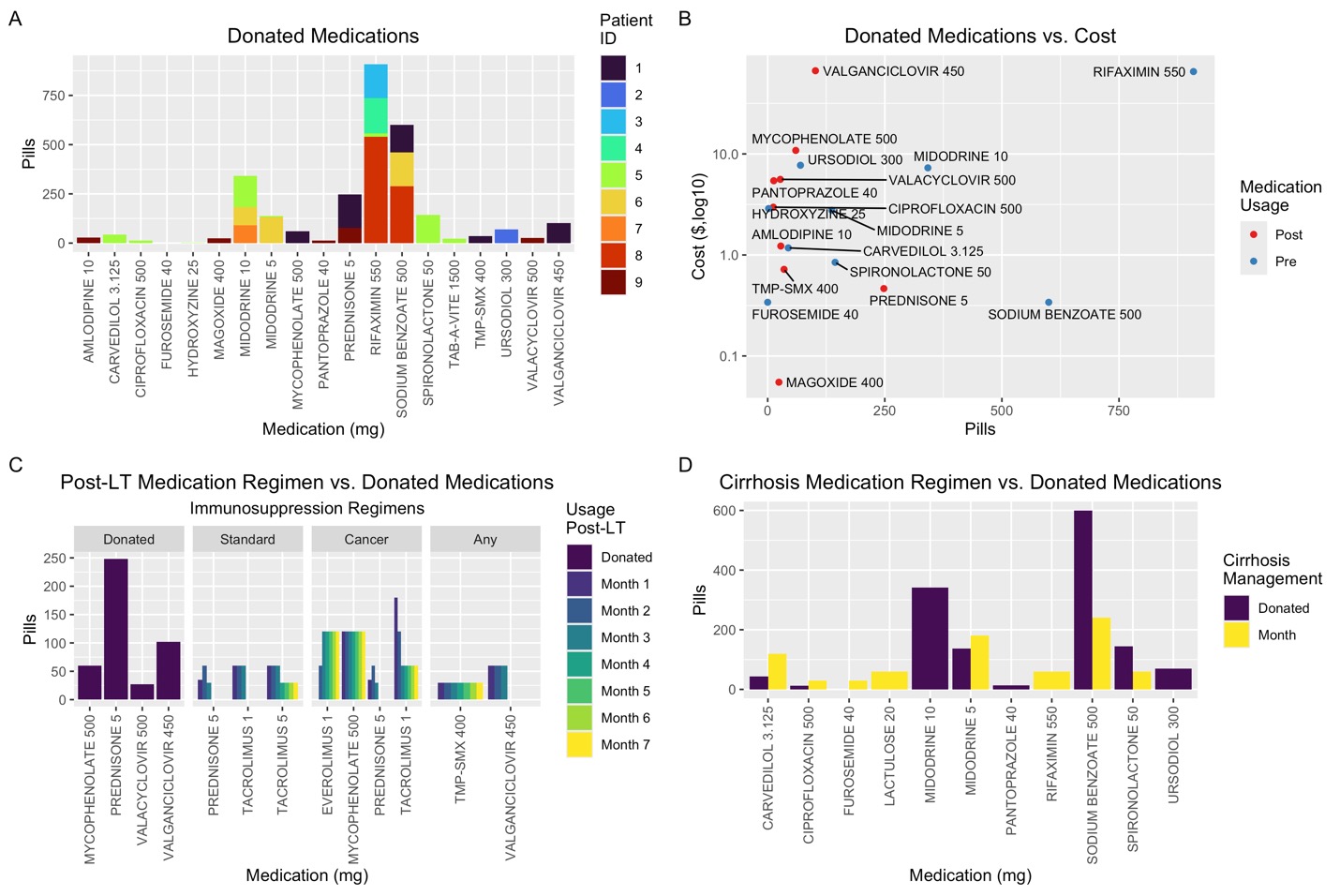
Methods: Patients were asked during routine scheduling calls to bring unused medications to their LT clinic appointment. Characteristics such as pill number, expiration, and tamper-evident seal were noted. Prices were sourced from UpToDate using the average of generic medication cost range. These pills were compared to a standard monthly regimen for a patient with cirrhosis and post-LT protocols. This project was formally determined to be quality improvement, not human subjects research, and was therefore not overseen by the Institutional Review Board, per institutional policy.
Results: Nine post-LT patients provided unused medications and were included in this pilot study. A total of 49 bottles with 17 different medications (Fig. 1A) were collected, worth $71,061.35 (Fig. 1B). Seven bottles were sealed and unexpired, each with 60 tabs of rifaximin 550 mg, worth $27,443. Four other bottles (1 of sodium benzoate, 4 of rifaximin) were unused but did not have an internal seal and were therefore still not donatable. Comparing all unused medications to monthly regimens for patients with cirrhosis or post-LT patients, the volumes of donated medications were sufficient for months of dosing of several medications, with potential to save thousands of dollars in costs (Figs. 1C, 1D, Table 1).
Discussion: This pilot study shows the potential for use of unused and donated medications to bridge care for patients who may have interrupted insurance coverage. Further work needs to understand how better to engage patients to donate unused medications, the scale of potential cost savings, and methods to broadly implement such practices.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yael Wollstein, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD. P4614 - Assessing the Role of Donated Medications in Post-Liver Transplant Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Chicago Medicine, Chicago, IL
Introduction: Significant financial toxicity is associated with chronic liver disease (CLD) and post-liver transplant (LT) care due to complex care needs including extensive medication regimens. This can pose a barrier to LT and even those with health insurance can suffer life-threatening gaps in coverage, with a patchwork of systems in place to mitigate the situation. However, given LT medication regimens are often dynamic based on a patient’s clinical situation, prescribed medications can go unused and be discarded. Illinois (IL) state law allows unopened and unexpired medications to be donated and reused. Donated medications have been used to fill gaps in insurance in other states and could be useful for patients with CLD. The aim of this study was to characterize the quantity and type of unused LT medications and determine whether they could be used for other patients.
Methods: Patients were asked during routine scheduling calls to bring unused medications to their LT clinic appointment. Characteristics such as pill number, expiration, and tamper-evident seal were noted. Prices were sourced from UpToDate using the average of generic medication cost range. These pills were compared to a standard monthly regimen for a patient with cirrhosis and post-LT protocols. This project was formally determined to be quality improvement, not human subjects research, and was therefore not overseen by the Institutional Review Board, per institutional policy.
Results: Nine post-LT patients provided unused medications and were included in this pilot study. A total of 49 bottles with 17 different medications (Fig. 1A) were collected, worth $71,061.35 (Fig. 1B). Seven bottles were sealed and unexpired, each with 60 tabs of rifaximin 550 mg, worth $27,443. Four other bottles (1 of sodium benzoate, 4 of rifaximin) were unused but did not have an internal seal and were therefore still not donatable. Comparing all unused medications to monthly regimens for patients with cirrhosis or post-LT patients, the volumes of donated medications were sufficient for months of dosing of several medications, with potential to save thousands of dollars in costs (Figs. 1C, 1D, Table 1).
Discussion: This pilot study shows the potential for use of unused and donated medications to bridge care for patients who may have interrupted insurance coverage. Further work needs to understand how better to engage patients to donate unused medications, the scale of potential cost savings, and methods to broadly implement such practices.
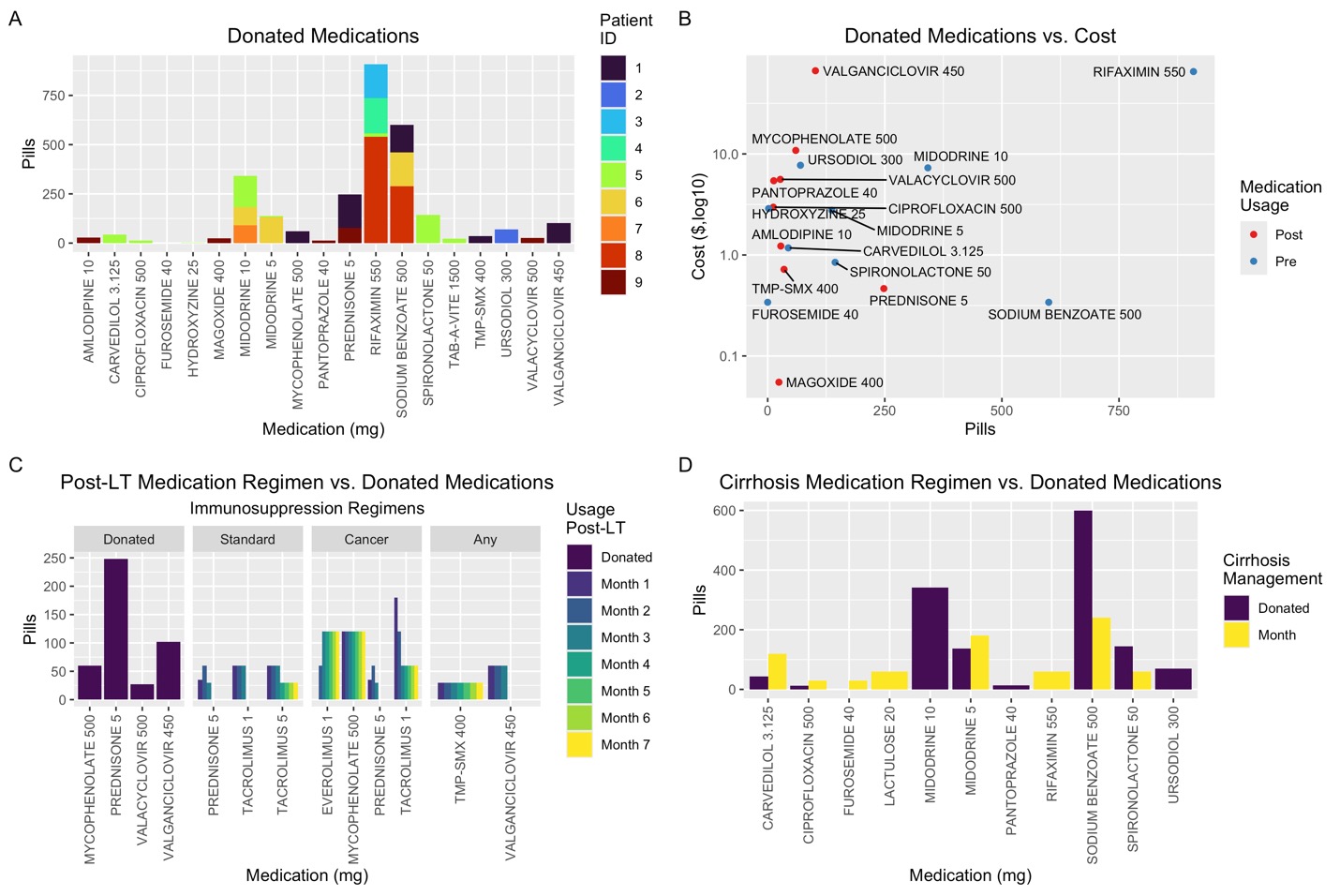
Figure: Figure 1. A) Donated medications by dose, colors indicating patients who donated. B) Donated medications by cost per pill, on a log-10 scale. C) Comparison of donated medications to standard post-liver transplant immunosuppression and infection prophylaxis regimens as per the University of Chicago standard protocol and post-malignancy protocols. D) Comparison of donated medication to a standard monthly regimen for a patient with cirrhosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yael Wollstein indicated no relevant financial relationships.
Sonali Paul: Intercept – Grant/Research Support. TARGET PharmaSolutions – Grant/Research Support.
Alan Hutchison indicated no relevant financial relationships.
Yael Wollstein, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD. P4614 - Assessing the Role of Donated Medications in Post-Liver Transplant Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
