Tuesday Poster Session
Category: Liver
P4617 - Extracorporeal Membrane Oxygenation Use in Patients Undergoing Allogenic Liver Transplant: A Retrospective National Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RV
Renuka Verma, MD
University of Nevada
Las Vegas, NV
Presenting Author(s)
Kyaw Min Tun, DO1, Renuka Verma, MD2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6
1Creighton University School of Medicine, Las Vegas, NV; 2University of Nevada, Las Vegas, NV; 3One Brooklyn Health-Interfaith Medical Center, New York, NY; 4Independent Researcher, Triolet, Pamplemousses, Mauritius; 5NYU Grossman School of Medicine, New York, NY; 6Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
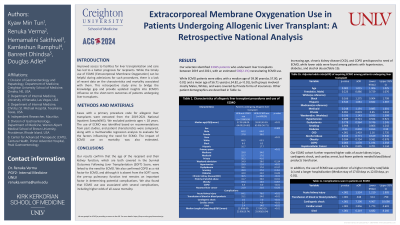
Introduction: Improved access to facilities for liver transplantation and care has led to a better prognosis for recipients. While the timely use of ECMO (Extracorporeal Membrane Oxygenation) can be helpful during admissions for such procedures, there is a lack of recent data on the characteristics and mortality associated with them. This retrospective study aims to bridge the knowledge gap and provide updated insights into ECMO’s influence on the short-term outcomes of patients undergoing liver transplants.
Methods: Cases with a primary procedure code for allogenic liver transplants were extracted from the 2019-2021 National Inpatient Sample(NIS). We excluded patients ages < 18 years. The use of ECMO was identified based on recommendations from past studies, and patient characteristics were compared, along with a multivariable regression analysis to evaluate for the factors influencing the need for ECMO. The impact of ECMO use on mortality was also estimated.
Results: Our selection identified 23365 patients who underwent liver transplants between 2019 and 2021, with an estimated 500(2.1%) necessitating ECMO use. While ECMO patients were older, with a median age of 59.00 years(vs.57.00, p< 0.01) and a mean age of 56.71 years(vs.54.82, p< 0.01), both groups involved mostly Males, Whites, and were covered by Private forms of insurances. Other patient demographics are described in Table 1a. Increasing age, chronic kidney disease (CKD), and COPD predisposed to need of ECMO, while lower odds were found among patients with hypertension, diabetes, and alcohol abuse(Table 1b). Our ECMO cohort further reported higher odds of acute kidney injury, cardiogenic shock, and cardiac arrest, but fewer patients needed blood/blood products transfusion. In addition, the use of ECMO was a predictor of a higher mortality rate(Table 1c) and a longer hospitalization (Median stay of 17.00 days vs.12.00 days, p< 0.01).
Discussion: Our results confirm that the age of the recipient and their kidney function, which are both covered in the Survival Outcomes Following Liver Transplantation (SOFT) Score, were linked to the need for ECMO. We also confirmed COPD as a risk factor for ECMO, and although it is absent from the SOFT score, the pre-op pulmonary function test remains an important factor in determining potential complications. We also found that ECMO use was associated with several complications, including higher odds of all-cause mortality.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyaw Min Tun, DO1, Renuka Verma, MD2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6. P4617 - Extracorporeal Membrane Oxygenation Use in Patients Undergoing Allogenic Liver Transplant: A Retrospective National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Las Vegas, NV; 2University of Nevada, Las Vegas, NV; 3One Brooklyn Health-Interfaith Medical Center, New York, NY; 4Independent Researcher, Triolet, Pamplemousses, Mauritius; 5NYU Grossman School of Medicine, New York, NY; 6Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Improved access to facilities for liver transplantation and care has led to a better prognosis for recipients. While the timely use of ECMO (Extracorporeal Membrane Oxygenation) can be helpful during admissions for such procedures, there is a lack of recent data on the characteristics and mortality associated with them. This retrospective study aims to bridge the knowledge gap and provide updated insights into ECMO’s influence on the short-term outcomes of patients undergoing liver transplants.
Methods: Cases with a primary procedure code for allogenic liver transplants were extracted from the 2019-2021 National Inpatient Sample(NIS). We excluded patients ages < 18 years. The use of ECMO was identified based on recommendations from past studies, and patient characteristics were compared, along with a multivariable regression analysis to evaluate for the factors influencing the need for ECMO. The impact of ECMO use on mortality was also estimated.
Results: Our selection identified 23365 patients who underwent liver transplants between 2019 and 2021, with an estimated 500(2.1%) necessitating ECMO use. While ECMO patients were older, with a median age of 59.00 years(vs.57.00, p< 0.01) and a mean age of 56.71 years(vs.54.82, p< 0.01), both groups involved mostly Males, Whites, and were covered by Private forms of insurances. Other patient demographics are described in Table 1a. Increasing age, chronic kidney disease (CKD), and COPD predisposed to need of ECMO, while lower odds were found among patients with hypertension, diabetes, and alcohol abuse(Table 1b). Our ECMO cohort further reported higher odds of acute kidney injury, cardiogenic shock, and cardiac arrest, but fewer patients needed blood/blood products transfusion. In addition, the use of ECMO was a predictor of a higher mortality rate(Table 1c) and a longer hospitalization (Median stay of 17.00 days vs.12.00 days, p< 0.01).
Discussion: Our results confirm that the age of the recipient and their kidney function, which are both covered in the Survival Outcomes Following Liver Transplantation (SOFT) Score, were linked to the need for ECMO. We also confirmed COPD as a risk factor for ECMO, and although it is absent from the SOFT score, the pre-op pulmonary function test remains an important factor in determining potential complications. We also found that ECMO use was associated with several complications, including higher odds of all-cause mortality.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyaw Min Tun indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Hemamalini Sakthivel indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Kyaw Min Tun, DO1, Renuka Verma, MD2, Hemamalini Sakthivel, MD3, Kamleshun Ramphul, MD4, Banreet Dhindsa, MD5, Douglas Adler, MD6. P4617 - Extracorporeal Membrane Oxygenation Use in Patients Undergoing Allogenic Liver Transplant: A Retrospective National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
