Tuesday Poster Session
Category: Liver
P4620 - Demographics, Outcomes, and Healthcare Utilization in Acute Liver Failure With Coma: A 5-Year Analysis From the National Readmission Database
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harshaman Kaur, MD
Mountain Vista Medical Center
Phoenix, AZ
Presenting Author(s)
Harshaman Kaur, MD1, Usman Rana, MD2, Afsheen Moshtaghi, DO3, Amninder Singh, MD4, Mankanwal S. Sachdev, MD5
1Mountain Vista Medical Center, Phoenix, AZ; 2The Wright Center for Graduate Medical Education, Scanton, PA; 3Verde Valley Medical Center, Cottonwood, AZ; 4The Wright Center for Graduate Medical Education, Scranton, PA; 5AZCDH, Paradise Valley, AZ
Introduction: Acute liver failure (ALF) with coma is a critical medical condition characterized by rapid deterioration of liver function, leading to high morbidity and mortality. Despite advances in medical care, the prognosis for patients with ALF remains poor. Understanding these patients' demographics, healthcare utilization, and outcomes is crucial for improving management strategies and healthcare policies. This study analyzes data from the National Readmission Database (NRD) from the Healthcare Cost and Utilization Project (HCUP) to identify trends, outcomes, and potential areas for intervention in patients diagnosed with ALF with coma.
Methods: We conducted a retrospective cohort study using the NRD from 2016 to 2020. Patients with a primary diagnosis of acute liver failure with coma were identified. Demographic data, length of stay, total charges, discharge disposition, mortality rates, and readmission rates were extracted. Yearly trends and patient characteristics, including gender, age, primary payor, and residence, were analyzed to assess patterns and outcomes over the study period.
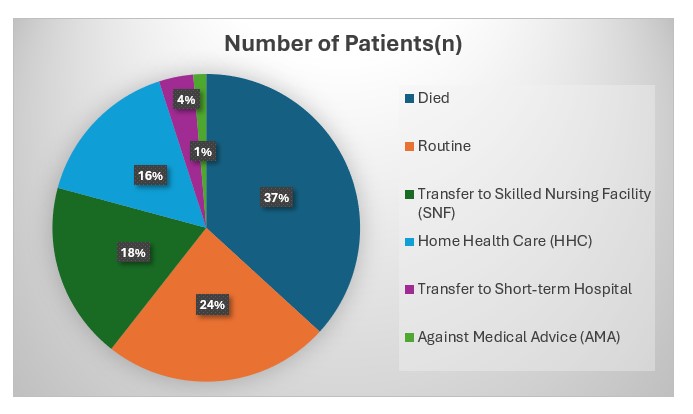
Results: A total of 2,223 patients with a primary diagnosis of acute liver failure with coma were identified from the NRD between 2016 and 2020. The median age of patients was 60.0 years (IQR: 16.0), with a median length of stay of 5 days (IQR: 8) and a median total charge of $56,575 (IQR: $107,913.5). Yearly admissions showed a declining trend: 739 in 2016 to 319 in 2020 as shown in Table 1. The gender distribution was almost even, with 1,162 females (52.3%) and 1,061 males (47.7%). The overall mortality rate was 36.7% (815 deaths). Among survivors, the discharge disposition is shown in Graph 1. The primary payors were Medicare (47.1%), Medicaid (24.1%), and private insurance (20.8%). Socioeconomic data indicated that 32.5% resided in the lowest income quartile. 14 patients were readmitted within 30 days, with 10 females and 4 males.
Discussion: This study highlights the significant burden of ALF with coma on healthcare systems, characterized by substantial mortality, and healthcare costs. Despite a declining trend in admissions, the high mortality rate underscores the critical nature of ALF. The substantial financial charges and varied discharge dispositions despite a low 30-day readmission rate, indicate a need for better resource allocation and post-discharge care planning. Further research should focus on early detection and innovative treatments to improve outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harshaman Kaur, MD1, Usman Rana, MD2, Afsheen Moshtaghi, DO3, Amninder Singh, MD4, Mankanwal S. Sachdev, MD5. P4620 - Demographics, Outcomes, and Healthcare Utilization in Acute Liver Failure With Coma: A 5-Year Analysis From the National Readmission Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mountain Vista Medical Center, Phoenix, AZ; 2The Wright Center for Graduate Medical Education, Scanton, PA; 3Verde Valley Medical Center, Cottonwood, AZ; 4The Wright Center for Graduate Medical Education, Scranton, PA; 5AZCDH, Paradise Valley, AZ
Introduction: Acute liver failure (ALF) with coma is a critical medical condition characterized by rapid deterioration of liver function, leading to high morbidity and mortality. Despite advances in medical care, the prognosis for patients with ALF remains poor. Understanding these patients' demographics, healthcare utilization, and outcomes is crucial for improving management strategies and healthcare policies. This study analyzes data from the National Readmission Database (NRD) from the Healthcare Cost and Utilization Project (HCUP) to identify trends, outcomes, and potential areas for intervention in patients diagnosed with ALF with coma.
Methods: We conducted a retrospective cohort study using the NRD from 2016 to 2020. Patients with a primary diagnosis of acute liver failure with coma were identified. Demographic data, length of stay, total charges, discharge disposition, mortality rates, and readmission rates were extracted. Yearly trends and patient characteristics, including gender, age, primary payor, and residence, were analyzed to assess patterns and outcomes over the study period.
Results: A total of 2,223 patients with a primary diagnosis of acute liver failure with coma were identified from the NRD between 2016 and 2020. The median age of patients was 60.0 years (IQR: 16.0), with a median length of stay of 5 days (IQR: 8) and a median total charge of $56,575 (IQR: $107,913.5). Yearly admissions showed a declining trend: 739 in 2016 to 319 in 2020 as shown in Table 1. The gender distribution was almost even, with 1,162 females (52.3%) and 1,061 males (47.7%). The overall mortality rate was 36.7% (815 deaths). Among survivors, the discharge disposition is shown in Graph 1. The primary payors were Medicare (47.1%), Medicaid (24.1%), and private insurance (20.8%). Socioeconomic data indicated that 32.5% resided in the lowest income quartile. 14 patients were readmitted within 30 days, with 10 females and 4 males.
Discussion: This study highlights the significant burden of ALF with coma on healthcare systems, characterized by substantial mortality, and healthcare costs. Despite a declining trend in admissions, the high mortality rate underscores the critical nature of ALF. The substantial financial charges and varied discharge dispositions despite a low 30-day readmission rate, indicate a need for better resource allocation and post-discharge care planning. Further research should focus on early detection and innovative treatments to improve outcomes.
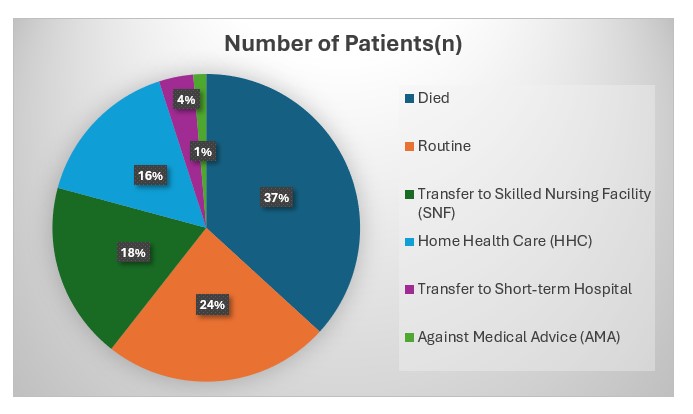
Figure: Graph 1: Discharge disposition of Acute Liver Failure (ALF) with Coma from the National Readmission Database, 2016-2020
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harshaman Kaur indicated no relevant financial relationships.
Usman Rana indicated no relevant financial relationships.
Afsheen Moshtaghi indicated no relevant financial relationships.
Amninder Singh indicated no relevant financial relationships.
Mankanwal Sachdev: Boston Scientific – Consultant. conmed – Consultant. Fuji – Consultant.
Harshaman Kaur, MD1, Usman Rana, MD2, Afsheen Moshtaghi, DO3, Amninder Singh, MD4, Mankanwal S. Sachdev, MD5. P4620 - Demographics, Outcomes, and Healthcare Utilization in Acute Liver Failure With Coma: A 5-Year Analysis From the National Readmission Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
