Tuesday Poster Session
Category: Liver
P4636 - A New 3-variable Model Outperforms MELD and King’s College Criteria in Hospitalized Patients With Severe Idiosyncratic DILI
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- AL
Alisa Likhitsup, MD
University of Michigan Medical School
Ann Arbor, MI
Presenting Author(s)
Alisa Likhitsup, MD1, Zemin Su, MS2, Jody A. rule, PhD3, Ashwin Rao, MD4, Valerie L. Durkalski-Mauldin, PhD2, William M. Lee, MD3, Robert Fontana, MD1
1University of Michigan Medical School, Ann Arbor, MI; 2Medical University of South Carolina, Charleston, SC; 3University of Texas Southwestern Medical Center, Dallas, TX; 4Baylor College of Medicine, Houston, TX
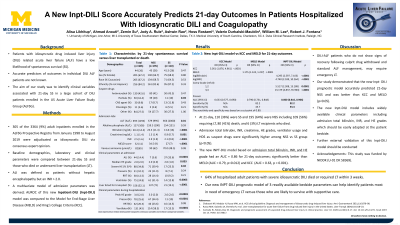
Introduction: Patients with non-acetaminophen related ALF including idiosyncratic drug induced liver injury (DILI) have a low likelihood of spontaneous survival (SS). However, accurate predictors of outcomes in individual DILI ALF patients are not known. The aim of our study was to identify clinical variables associated with 21-day SS in a large cohort of DILI-ALI/ALF patients prospectively enrolled in the US Acute Liver Failure Study Group (ALFSG).
Methods: 305 of the 3364 adult patients enrolled in the ALFSG Registry from Jan 1998 to August 2019 were adjudicated as idiosyncratic DILI via expert opinion. Baseline demographics and clinical parameters including hepatic encephalopathy (HE) grades, vasopressor, ventilator use, and admission laboratory values were compared between 21-day SS and those who died or underwent liver transplantation (LT). ALI was defined as patients without HE but an INR > 2.0. The AUROC of a multivariate logistic regression model was compared to the Model for End-Stage Liver Disease (MELD) and King’s College Criteria scores.
Results: 44 patients had ALI- DILI (HE grade 0) and 261 had ALF-DILI (HE grade 1-4) attributed to 230 individual agents (36% antimicrobials, 23% HDS, 13% CNS agents, 4% oncologic/biologic agents, 24% other). Median age was 44 years, 67% were female, and median MELD scores were 32. At 3 weeks, there were 110 (36%) SS and 195 (64%) non-spontaneous survival (NSS) including 109 (56%) requiring LT, 80 (41%) death, and 6 (3%) LT recipients who died. Admission total bilirubin, INR, creatinine, HE grades, and ventilator usage were significantly higher among NSS vs SS group (p< 0.05) (Table 1). Antimicrobials were more common among SS (p< 0.01). Other suspect drug classes did not differ between the 2 groups. A new 3-variable model based on admission total bilirubin, INR, and HE grade had an AUC = 0.86 (95% CI 0.82 – 0.90), significantly better than MELD (AUC = 0.79; 95% CI 0.73 – 0.85, p=0.012) and King’s College Criteria (AUC = 0.63; 95% CI 0.58 – 0.69, p < 0.001) in predicting SS.
Discussion: Nearly 66% of hospitalized patients with severe idiosyncratic DILI died or required LT within 3 weeks. A new prognostic model of 3 readily available clinical parameters (total bilirubin, INR, HE grades) can help identify patients most in need of emergency LT versus those likely to survive with supportive care. This model was superior to MELD and King’s College in identifying non-survivors with DILI related ALI/ALF.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alisa Likhitsup, MD1, Zemin Su, MS2, Jody A. rule, PhD3, Ashwin Rao, MD4, Valerie L. Durkalski-Mauldin, PhD2, William M. Lee, MD3, Robert Fontana, MD1. P4636 - A New 3-variable Model Outperforms MELD and King’s College Criteria in Hospitalized Patients With Severe Idiosyncratic DILI, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan Medical School, Ann Arbor, MI; 2Medical University of South Carolina, Charleston, SC; 3University of Texas Southwestern Medical Center, Dallas, TX; 4Baylor College of Medicine, Houston, TX
Introduction: Patients with non-acetaminophen related ALF including idiosyncratic drug induced liver injury (DILI) have a low likelihood of spontaneous survival (SS). However, accurate predictors of outcomes in individual DILI ALF patients are not known. The aim of our study was to identify clinical variables associated with 21-day SS in a large cohort of DILI-ALI/ALF patients prospectively enrolled in the US Acute Liver Failure Study Group (ALFSG).
Methods: 305 of the 3364 adult patients enrolled in the ALFSG Registry from Jan 1998 to August 2019 were adjudicated as idiosyncratic DILI via expert opinion. Baseline demographics and clinical parameters including hepatic encephalopathy (HE) grades, vasopressor, ventilator use, and admission laboratory values were compared between 21-day SS and those who died or underwent liver transplantation (LT). ALI was defined as patients without HE but an INR > 2.0. The AUROC of a multivariate logistic regression model was compared to the Model for End-Stage Liver Disease (MELD) and King’s College Criteria scores.
Results: 44 patients had ALI- DILI (HE grade 0) and 261 had ALF-DILI (HE grade 1-4) attributed to 230 individual agents (36% antimicrobials, 23% HDS, 13% CNS agents, 4% oncologic/biologic agents, 24% other). Median age was 44 years, 67% were female, and median MELD scores were 32. At 3 weeks, there were 110 (36%) SS and 195 (64%) non-spontaneous survival (NSS) including 109 (56%) requiring LT, 80 (41%) death, and 6 (3%) LT recipients who died. Admission total bilirubin, INR, creatinine, HE grades, and ventilator usage were significantly higher among NSS vs SS group (p< 0.05) (Table 1). Antimicrobials were more common among SS (p< 0.01). Other suspect drug classes did not differ between the 2 groups. A new 3-variable model based on admission total bilirubin, INR, and HE grade had an AUC = 0.86 (95% CI 0.82 – 0.90), significantly better than MELD (AUC = 0.79; 95% CI 0.73 – 0.85, p=0.012) and King’s College Criteria (AUC = 0.63; 95% CI 0.58 – 0.69, p < 0.001) in predicting SS.
Discussion: Nearly 66% of hospitalized patients with severe idiosyncratic DILI died or required LT within 3 weeks. A new prognostic model of 3 readily available clinical parameters (total bilirubin, INR, HE grades) can help identify patients most in need of emergency LT versus those likely to survive with supportive care. This model was superior to MELD and King’s College in identifying non-survivors with DILI related ALI/ALF.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alisa Likhitsup indicated no relevant financial relationships.
Zemin Su indicated no relevant financial relationships.
Jody rule indicated no relevant financial relationships.
Ashwin Rao indicated no relevant financial relationships.
Valerie Durkalski-Mauldin indicated no relevant financial relationships.
William Lee: Akero – Grant/Research Support. Camurus – Grant/Research Support. Genentech – Consultant. Gilead – Grant/Research Support. GSK – Consultant. Lipocine – Grant/Research Support. RAPT – Consultant. SeaGen – Consultant. Veristat – Consultant.
Robert Fontana: Kezar Pharmaceuticals – Grant/Research Support. Takeda Pharmaceuticals – Grant/Research Support.
Alisa Likhitsup, MD1, Zemin Su, MS2, Jody A. rule, PhD3, Ashwin Rao, MD4, Valerie L. Durkalski-Mauldin, PhD2, William M. Lee, MD3, Robert Fontana, MD1. P4636 - A New 3-variable Model Outperforms MELD and King’s College Criteria in Hospitalized Patients With Severe Idiosyncratic DILI, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
