Tuesday Poster Session
Category: Liver
P4642 - Patients Admitted With Sepsis and Gastrointestinal Bleeding, Affected by Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), Exhibit Worse Clinical Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhamad Oum, MD
Saint Agnes Medical Center
Fresno, CA
Presenting Author(s)
Muhamad Oum, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Khalid Aloum, MD4, Sandeep Sekhon, MD1
1Saint Agnes Medical Center, Fresno, CA; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo Health Sciences Campus, Toledo, OH; 4St. Barnabas Hospital, Bronx, NY
Introduction: The association between sepsis and gastrointestinal bleeding (GIB) is complex and multifactorial. In the presence of MASLD, the risk of complications during sepsis, including bleeding, may increase due to compromised liver function. Limited scientific evidence exists examining outcomes among MASLD patients presenting with sepsis and GIB. Our objective was to assess clinical outcomes in this population.
Methods: We analyzed the National Inpatient Sample from 2017-2020 to identify adult patients with MASLD hospitalized due to sepsis and GIB. The primary endpoint was inpatient mortality, with secondary endpoints including cardiogenic shock, intubation, length of stay (LOS), and total hospital charges. Multivariable logistic regression analysis was used to estimate clinical outcomes, with significance set at P< 0.05.
Results: We identified 294,585 hospitalizations with sepsis and GIB, among which 59,344 (20.1%) had a diagnosis of MASLD. Comparing MASLD and Non-MASLD cohorts, the mean age was 59.6 vs 62.8 years, males constituted 56.6% vs 56%, and White ethnicity accounted for 59.6% vs 62.8%. The prevalence of obesity was 13.2% vs 13.4%, diabetes mellitus (DM) was 30% vs 36%, chronic obstructive pulmonary disease (COPD) was 19.5% vs 22.3%, dyslipidemia was 20.6% vs 31%, atrial fibrillation (AFIB) was 24% vs 29.6%, hypertension (HTN) was 18.1% vs 22.4%, heart failure (HF) was 32.1% vs 34.3%, peripheral vascular disease (PVD) was 2% vs 3.4%, anemia was 20.1% vs 22.7%, acute kidney injury (AKI) was 82.1% vs 69.2% and chronic kidney disease (CKD) was 29.6% vs 34.1%.
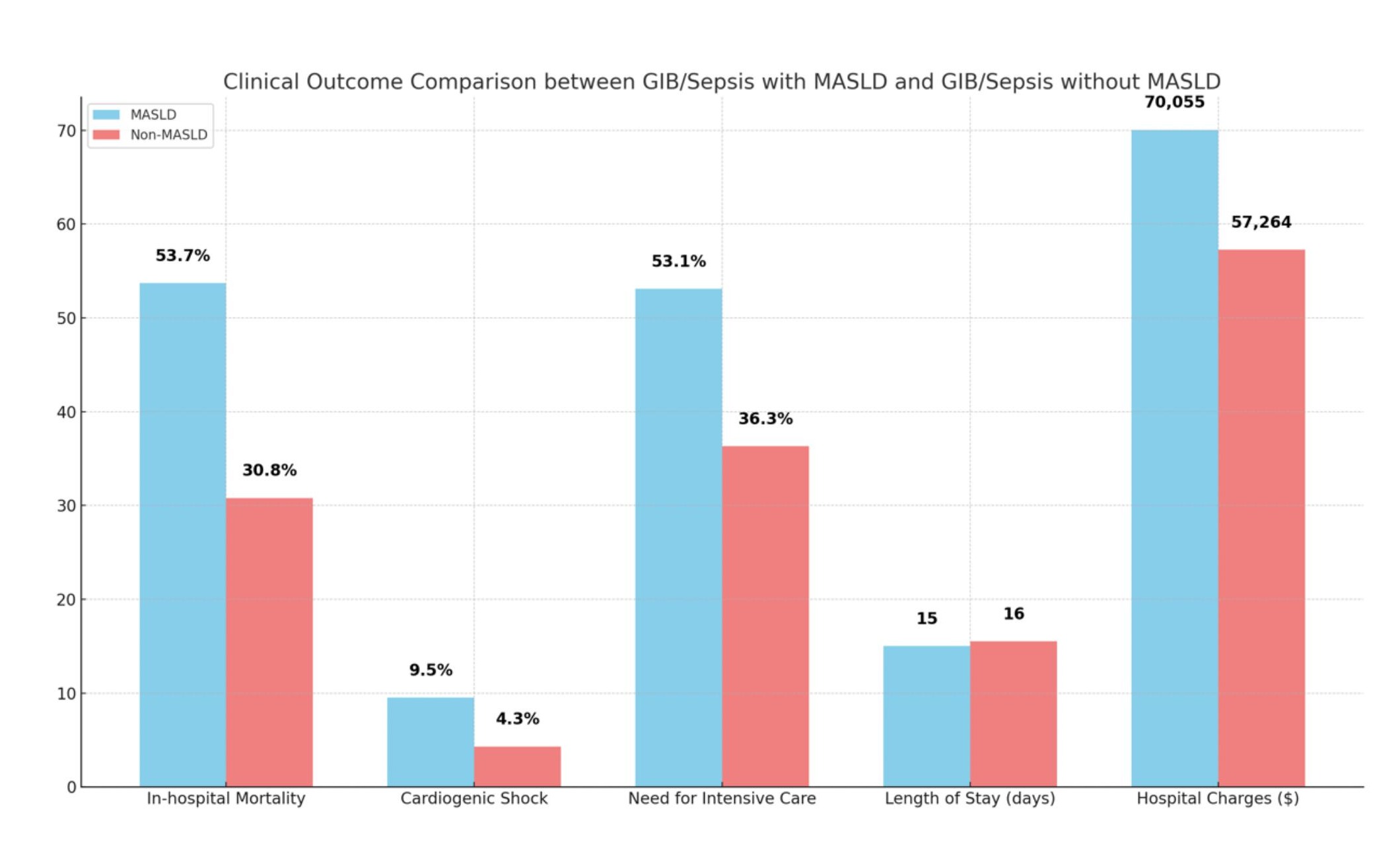
Clinical outcomes differed significantly between MASLD and Non-MASLD cohorts: in-hospital mortality rates were 53.7% vs 30.8%, with an odds ratio (OR) of 2.7 (CI 2.6-2.8); rates of cardiogenic shock were 9.5% vs 4.3% (OR 2.1, CI 1.9-2.3); need for intensive care was 53.1% vs 36.3% with an OR of 1.8 (CI 1.7-1.8); LOS was 15 days vs 15.5 days (IRR 0.86, CI 0.83-0.88); and hospital charges were $70,055 vs $57,264 (IRR 1.06, CI 1.02-1.1). All comparisons had a p-value< 0.001 and were adjusted for age, sex, race, comorbidity indices, obesity, AFIB, DM, HTN, PVD, AKI, CKD, and stroke.
Discussion: The MASLD cohort, though younger showed significantly worse clinical outcomes despite lower rates of all mentioned comorbidities except for higher rates of AKI. This suggests MASLD is a negative predictor when patients present with sepsis and GIB, leading to higher mortality rates, rates of cardiogenic shock, and increased resource utilization.
Disclosures:
Muhamad Oum, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Khalid Aloum, MD4, Sandeep Sekhon, MD1. P4642 - Patients Admitted With Sepsis and Gastrointestinal Bleeding, Affected by Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), Exhibit Worse Clinical Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Agnes Medical Center, Fresno, CA; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo Health Sciences Campus, Toledo, OH; 4St. Barnabas Hospital, Bronx, NY
Introduction: The association between sepsis and gastrointestinal bleeding (GIB) is complex and multifactorial. In the presence of MASLD, the risk of complications during sepsis, including bleeding, may increase due to compromised liver function. Limited scientific evidence exists examining outcomes among MASLD patients presenting with sepsis and GIB. Our objective was to assess clinical outcomes in this population.
Methods: We analyzed the National Inpatient Sample from 2017-2020 to identify adult patients with MASLD hospitalized due to sepsis and GIB. The primary endpoint was inpatient mortality, with secondary endpoints including cardiogenic shock, intubation, length of stay (LOS), and total hospital charges. Multivariable logistic regression analysis was used to estimate clinical outcomes, with significance set at P< 0.05.
Results: We identified 294,585 hospitalizations with sepsis and GIB, among which 59,344 (20.1%) had a diagnosis of MASLD. Comparing MASLD and Non-MASLD cohorts, the mean age was 59.6 vs 62.8 years, males constituted 56.6% vs 56%, and White ethnicity accounted for 59.6% vs 62.8%. The prevalence of obesity was 13.2% vs 13.4%, diabetes mellitus (DM) was 30% vs 36%, chronic obstructive pulmonary disease (COPD) was 19.5% vs 22.3%, dyslipidemia was 20.6% vs 31%, atrial fibrillation (AFIB) was 24% vs 29.6%, hypertension (HTN) was 18.1% vs 22.4%, heart failure (HF) was 32.1% vs 34.3%, peripheral vascular disease (PVD) was 2% vs 3.4%, anemia was 20.1% vs 22.7%, acute kidney injury (AKI) was 82.1% vs 69.2% and chronic kidney disease (CKD) was 29.6% vs 34.1%.
Clinical outcomes differed significantly between MASLD and Non-MASLD cohorts: in-hospital mortality rates were 53.7% vs 30.8%, with an odds ratio (OR) of 2.7 (CI 2.6-2.8); rates of cardiogenic shock were 9.5% vs 4.3% (OR 2.1, CI 1.9-2.3); need for intensive care was 53.1% vs 36.3% with an OR of 1.8 (CI 1.7-1.8); LOS was 15 days vs 15.5 days (IRR 0.86, CI 0.83-0.88); and hospital charges were $70,055 vs $57,264 (IRR 1.06, CI 1.02-1.1). All comparisons had a p-value< 0.001 and were adjusted for age, sex, race, comorbidity indices, obesity, AFIB, DM, HTN, PVD, AKI, CKD, and stroke.
Discussion: The MASLD cohort, though younger showed significantly worse clinical outcomes despite lower rates of all mentioned comorbidities except for higher rates of AKI. This suggests MASLD is a negative predictor when patients present with sepsis and GIB, leading to higher mortality rates, rates of cardiogenic shock, and increased resource utilization.
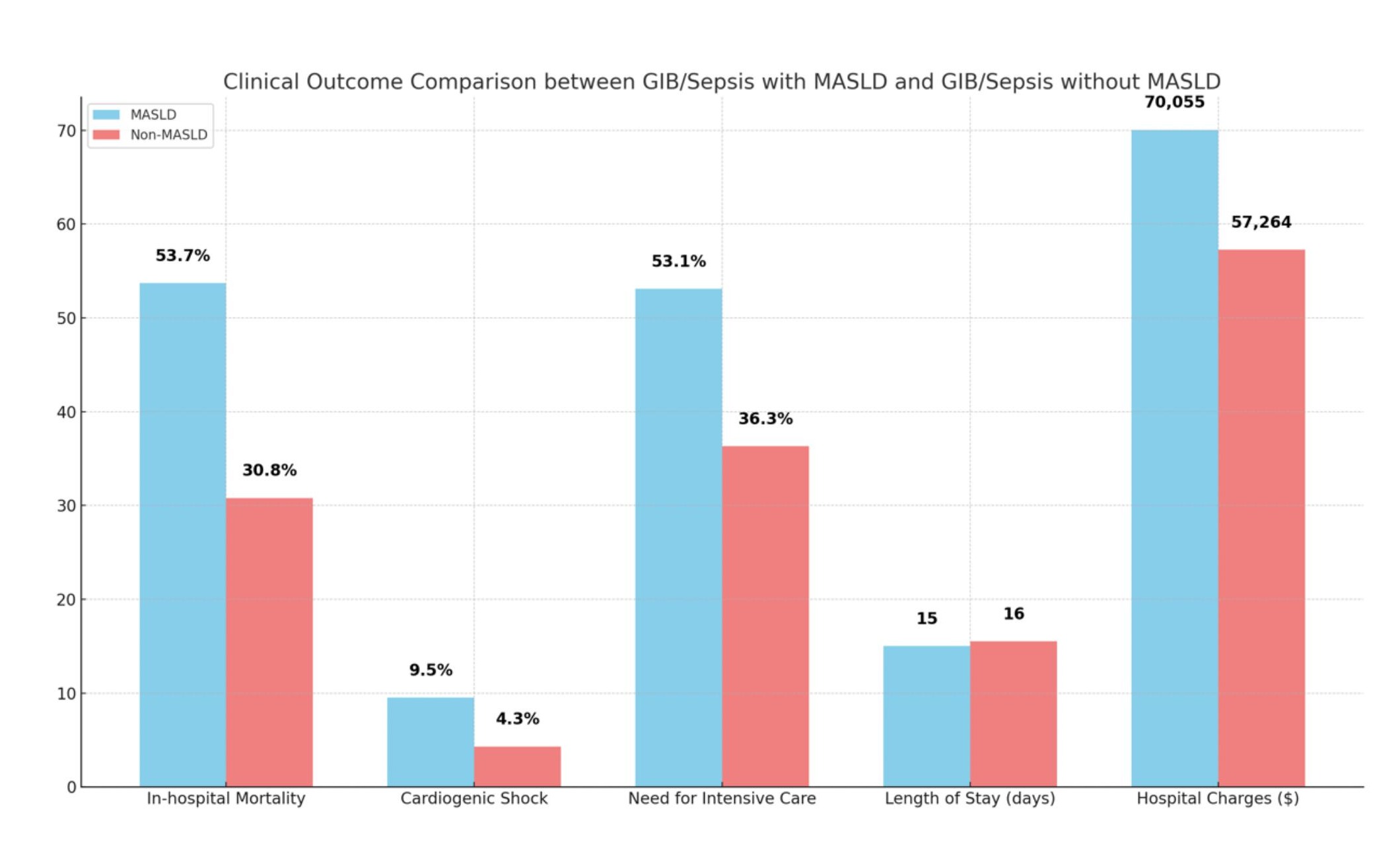
Figure: Outcomes stratified by presence of MASLD.
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Khalid Aloum indicated no relevant financial relationships.
Sandeep Sekhon indicated no relevant financial relationships.
Muhamad Oum, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Khalid Aloum, MD4, Sandeep Sekhon, MD1. P4642 - Patients Admitted With Sepsis and Gastrointestinal Bleeding, Affected by Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), Exhibit Worse Clinical Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
