Tuesday Poster Session
Category: Liver
P4654 - Palliative Care Utilization in Alcoholic Cirrhosis Admissions: Insights from a Six-Year US National Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Sania Saleem, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daksh Ahluwalia, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Kathmandu, Bagmati, Nepal
Introduction: Alcoholic Cirrhosis (AC) contributes significantly to global disease burden. Despite numerous advancements in management options, outcomes for patients with AC remain challenging, with substantial morbidity and mortality. Palliative care consultations (PCC) are essential in symptom management and improving communication about patient’s goals in such cases. This study aims to explore the utilization of PCC in patients admitted for AC.
Methods: This retrospective analysis used the National Inpatient Sample 2016 through 2021. The study included admissions for AC identified using the International Classification of Diseases, 10th revision (ICD) codes. Similarly, PCC was identified using ICD codes. Statistical analysis was done using multivariable logistic regression. The longitudinal trends of AC and PCC were also analyzed. A P-value of < 0.05 was considered statistically significant.
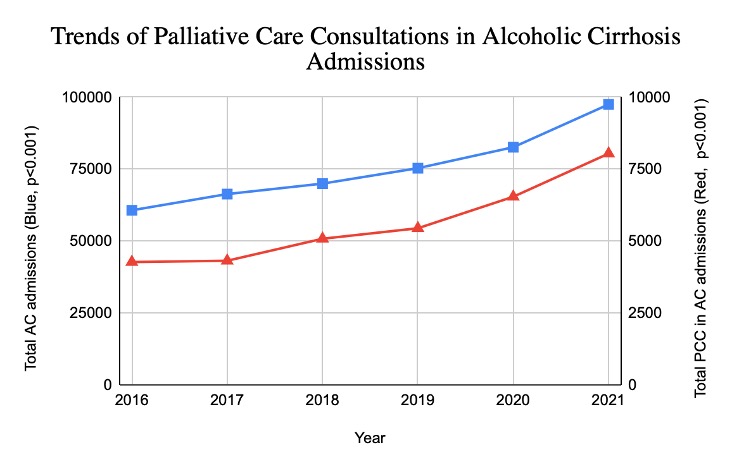
Results: There were 452,450 admissions for AC, with 33,690 (7.46%) admissions involving PCC. Patients receiving PCC were older (mean age 56 years vs. 53 years, p < 0.001) and had a longer length of stay (10 days vs. 6 days, p < 0.001) compared to total AC admissions. Hispanics had lower odds of PCC compared to whites (OR 0.71, p< 0.001). PCC was more common in patients with higher Charlson Comorbidity Index (CCI) (OR 2.99 for CCI ≥ 3, p < 0.001). Patients admitted to metropolitan teaching hospitals had higher odds of PCC than non-metropolitan hospitals (OR 1.22, p< 0.001). Those with Medicaid had higher odds of PCC than Medicaid patients (OR 1.13, p< 0.003). Trend analysis showed a significant increase in AC admissions and PCC among such admissions.
Discussion: These findings demonstrate increasing utilization of palliative care services in the management of AC, particularly in older patients and those with higher co-morbidities. Medicare patients are typically older than Medicaid patients, so the higher incidence of PCC may be related to their age demographics. The geographic and institutional variability in PCC may be related to the differences in the availability of resources and local policies across regions and institutions. Ae of PCC in Hispanics may be related to provider biases or differences in cultural attitudes, making them less likely to opt for or receive PCC. Although there has been an increasing trend in PCC among AC patients, disparities persist among different subsets. Thus, further research is needed to develop strategies that ensure equitable palliative care services for all subgroups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota, MD1, Sania Saleem, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daksh Ahluwalia, MD1. P4654 - Palliative Care Utilization in Alcoholic Cirrhosis Admissions: Insights from a Six-Year US National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Kathmandu, Bagmati, Nepal
Introduction: Alcoholic Cirrhosis (AC) contributes significantly to global disease burden. Despite numerous advancements in management options, outcomes for patients with AC remain challenging, with substantial morbidity and mortality. Palliative care consultations (PCC) are essential in symptom management and improving communication about patient’s goals in such cases. This study aims to explore the utilization of PCC in patients admitted for AC.
Methods: This retrospective analysis used the National Inpatient Sample 2016 through 2021. The study included admissions for AC identified using the International Classification of Diseases, 10th revision (ICD) codes. Similarly, PCC was identified using ICD codes. Statistical analysis was done using multivariable logistic regression. The longitudinal trends of AC and PCC were also analyzed. A P-value of < 0.05 was considered statistically significant.
Results: There were 452,450 admissions for AC, with 33,690 (7.46%) admissions involving PCC. Patients receiving PCC were older (mean age 56 years vs. 53 years, p < 0.001) and had a longer length of stay (10 days vs. 6 days, p < 0.001) compared to total AC admissions. Hispanics had lower odds of PCC compared to whites (OR 0.71, p< 0.001). PCC was more common in patients with higher Charlson Comorbidity Index (CCI) (OR 2.99 for CCI ≥ 3, p < 0.001). Patients admitted to metropolitan teaching hospitals had higher odds of PCC than non-metropolitan hospitals (OR 1.22, p< 0.001). Those with Medicaid had higher odds of PCC than Medicaid patients (OR 1.13, p< 0.003). Trend analysis showed a significant increase in AC admissions and PCC among such admissions.
Discussion: These findings demonstrate increasing utilization of palliative care services in the management of AC, particularly in older patients and those with higher co-morbidities. Medicare patients are typically older than Medicaid patients, so the higher incidence of PCC may be related to their age demographics. The geographic and institutional variability in PCC may be related to the differences in the availability of resources and local policies across regions and institutions. Ae of PCC in Hispanics may be related to provider biases or differences in cultural attitudes, making them less likely to opt for or receive PCC. Although there has been an increasing trend in PCC among AC patients, disparities persist among different subsets. Thus, further research is needed to develop strategies that ensure equitable palliative care services for all subgroups.
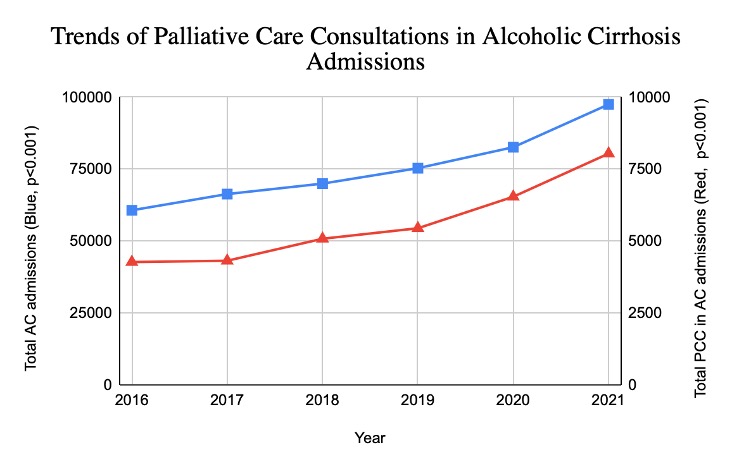
Figure: Trends in Palliative Care Consultations among Alcoholic Cirrhosis Admissions
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Sania Saleem indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Daksh Ahluwalia indicated no relevant financial relationships.
Abhin Sapkota, MD1, Sania Saleem, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daksh Ahluwalia, MD1. P4654 - Palliative Care Utilization in Alcoholic Cirrhosis Admissions: Insights from a Six-Year US National Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
