Tuesday Poster Session
Category: Liver
P4655 - Suboptimal Adherence to Guidelines to Non-Invasively Rule Out Esophageal Varices In Austin, Texas
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- NG
Nikitha Gangasani, MD
University of Texas at Austin Dell Medical School
Austin, TX
Presenting Author(s)
Nikitha Gangasani, MD, Sagarika Satyavada, MD, Christoffer Lam, MD
University of Texas at Austin Dell Medical School, Austin, TX
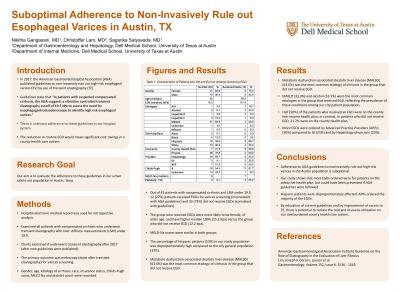
Introduction: In 2017, the American Gastroenterological Association (AGA) published guidelines to non-invasively rule out high-risk esophageal varices (EV) by use of transient elastography (TE). The reduction in routine EGD would mean significant cost savings in a county health care system. Our aim is to evaluate the adherence to these guidelines in our urban safety-net population in Austin, Texas.
Methods: We included all patients with compensated cirrhosis who underwent TE with liver stiffness measurements (LSM) under 19.5 from 2017 to present. The primary outcome was endoscopy (done after TE) for varices screening. Gender, age, etiology of cirrhosis, race, insurance status, Childs-Pugh score, MELD-Na and platelet count were recorded.
Results: Out of 45 patients with compensated cirrhosis and LSM under 19.5, 12 (27%) patients received EGDs for varices screening (inconsistent with AGA guidelines) and 33 (73%) did not receive EGDs (consistent with guidelines). The group who received EGDs were more likely to be female, of older age, and have higher median LSMs (15.2 kpa) versus the group who did not receive EGD (12.2 kpa). MELD-Na scores were similar in both groups. The percentage of Hispanic patients (53%) in our study population was disproportionately high compared to the city general population (33%). Metabolic dysfunction-associated steatotic liver disease (MALSD) (63.6%) was the most common etiology of cirrhosis in the group that did not receive EGD. MASLD (33.3%) and alcohol (33.3%) were the most common etiologies in the group that received EGD, reflecting the prevalence of these conditions among our city patient population. Half (50%) of the patients who received an EGD were on the county low-income health plan; in contrast, in patients who did not receive EGD, 21.2% were on the county health plan. More EGDs were ordered by Advanced Practice Providers (APPs) (50%) compared to GI (25%) and by Hepatology physicians (25%).
Discussion: Adherence to AGA guidelines to noninvasively rule out high-risk varices in the Austin population is suboptimal. Our study shows that most EGDs ordered were for patients on the safety net health plan, but could have been prevented if AGA guidelines were followed. Hispanic patients were disproportionately affected. APPs ordered the majority of the EGDs. By education of current guidelines and by improvement of access to TE, there is potential to reduce the cost and resource utilization on our overburdened county health care system.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nikitha Gangasani, MD, Sagarika Satyavada, MD, Christoffer Lam, MD. P4655 - Suboptimal Adherence to Guidelines to Non-Invasively Rule Out Esophageal Varices In Austin, Texas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas at Austin Dell Medical School, Austin, TX
Introduction: In 2017, the American Gastroenterological Association (AGA) published guidelines to non-invasively rule out high-risk esophageal varices (EV) by use of transient elastography (TE). The reduction in routine EGD would mean significant cost savings in a county health care system. Our aim is to evaluate the adherence to these guidelines in our urban safety-net population in Austin, Texas.
Methods: We included all patients with compensated cirrhosis who underwent TE with liver stiffness measurements (LSM) under 19.5 from 2017 to present. The primary outcome was endoscopy (done after TE) for varices screening. Gender, age, etiology of cirrhosis, race, insurance status, Childs-Pugh score, MELD-Na and platelet count were recorded.
Results: Out of 45 patients with compensated cirrhosis and LSM under 19.5, 12 (27%) patients received EGDs for varices screening (inconsistent with AGA guidelines) and 33 (73%) did not receive EGDs (consistent with guidelines). The group who received EGDs were more likely to be female, of older age, and have higher median LSMs (15.2 kpa) versus the group who did not receive EGD (12.2 kpa). MELD-Na scores were similar in both groups. The percentage of Hispanic patients (53%) in our study population was disproportionately high compared to the city general population (33%). Metabolic dysfunction-associated steatotic liver disease (MALSD) (63.6%) was the most common etiology of cirrhosis in the group that did not receive EGD. MASLD (33.3%) and alcohol (33.3%) were the most common etiologies in the group that received EGD, reflecting the prevalence of these conditions among our city patient population. Half (50%) of the patients who received an EGD were on the county low-income health plan; in contrast, in patients who did not receive EGD, 21.2% were on the county health plan. More EGDs were ordered by Advanced Practice Providers (APPs) (50%) compared to GI (25%) and by Hepatology physicians (25%).
Discussion: Adherence to AGA guidelines to noninvasively rule out high-risk varices in the Austin population is suboptimal. Our study shows that most EGDs ordered were for patients on the safety net health plan, but could have been prevented if AGA guidelines were followed. Hispanic patients were disproportionately affected. APPs ordered the majority of the EGDs. By education of current guidelines and by improvement of access to TE, there is potential to reduce the cost and resource utilization on our overburdened county health care system.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nikitha Gangasani indicated no relevant financial relationships.
Sagarika Satyavada indicated no relevant financial relationships.
Christoffer Lam indicated no relevant financial relationships.
Nikitha Gangasani, MD, Sagarika Satyavada, MD, Christoffer Lam, MD. P4655 - Suboptimal Adherence to Guidelines to Non-Invasively Rule Out Esophageal Varices In Austin, Texas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
