Tuesday Poster Session
Category: Liver
P4662 - Treatment Persistence and ALP Normalization Among Patients With Primary Biliary Cholangitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CM
C. Fiorella Murillo Perez, PhD
Gilead Sciences, Inc.
Foster City, CA
Presenting Author(s)
Kris V.. Kowdley, MD, FACG1, Jonathan Ieyoub, MS, NP2, Yi Pan, PhD3, Mihail Samnaliev, PhD3, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD2
1Liver Institute Northwest, Seattle, WA; 2Gilead Sciences, Inc., Foster City, CA; 3Stratevi, Boston, MA; 4Stratevi, Santa Monica, CA
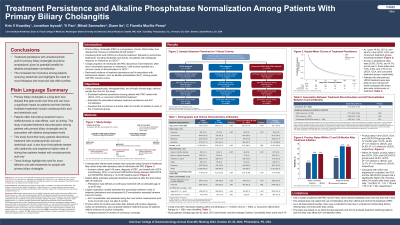
Introduction: Primary biliary cholangitis (PBC) is a progressive chronic inflammatory liver disease. Ursodeoxycholic acid (UDCA) is a first-line treatment, while obeticholic acid (OCA) is reserved as an add-on therapy for patients with inadequate response or intolerance to UDCA. We evaluated persistence of these therapies among individuals with PBC and its association with ALP normalization in real world settings in the U.S.
Methods: A retrospective intent-to-treat analysis was conducted using Komodo’s Healthcare Map claims linked with laboratory data of individuals with PBC aged ≥18 years, who started UDCA monotherapy, OCA, or concurrent UDCA/OCA therapy between 09/01/2018 and 09/30/2023 following a 12-month baseline period. Kaplan-Meier estimates assessed treatment persistence after start (index) date of treatment, defined as continuous treatment with an allowable gap of up to 60 days. Logistic regression models estimated the association between a lack of treatment persistence and subsequent ALP normalization (Quest thresholds) assessed between 6-24 months. Pruritus within 24 months post-index, defined with pruritus diagnosis codes and treatments, was compared among treatment groups using logistic regression models. Analyses required 24 months of continuous coverage.
Results: A total of 19,003, 1,903 and 1,581 people with PBC were treated with UDCA, OCA, and concurrent UDCA/OCA, respectively. Study participants’ average age was 62 years, 87% were female and their average Charlson Comorbidity Index was 4.9. At one year, only 42% remained persistent on UDCA, 33% on OCA, and 46% on concurrent OCA/UDCA. In a subgroup of patients (N=2,156) with an ALP test between 6-24 months post index and treated with UDCA, lack of treatment persistence was associated with lower odds of ALP normalization (OR 0.77 [95% CI 0.63-0.93] (Table 1). Pruritus rates in the UDCA, OCA, and OCA/UDCA groups within 24 months were 20.8%, 32.5% (p< .01 relative to UDCA), and 32.1% (p< .01 relative to UDCA), respectively. Compared to UDCA and adjusting for covariates, the OCA and the OCA/UDCA groups had a higher risk of pruritus within 24 months after index (OR 1.54 [95% CI 1.33, 1.79] and 1.55 [1.32, 1.82], respectively).
Discussion: Remaining persistent with UDCA treatment among individuals with PBC should be emphasized, given its potential benefits for ALP normalization. The increased risk of pruritus among patients receiving OCA highlights the need for novel therapies with improved side effect profiles.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kris V.. Kowdley, MD, FACG1, Jonathan Ieyoub, MS, NP2, Yi Pan, PhD3, Mihail Samnaliev, PhD3, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD2. P4662 - Treatment Persistence and ALP Normalization Among Patients With Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Liver Institute Northwest, Seattle, WA; 2Gilead Sciences, Inc., Foster City, CA; 3Stratevi, Boston, MA; 4Stratevi, Santa Monica, CA
Introduction: Primary biliary cholangitis (PBC) is a progressive chronic inflammatory liver disease. Ursodeoxycholic acid (UDCA) is a first-line treatment, while obeticholic acid (OCA) is reserved as an add-on therapy for patients with inadequate response or intolerance to UDCA. We evaluated persistence of these therapies among individuals with PBC and its association with ALP normalization in real world settings in the U.S.
Methods: A retrospective intent-to-treat analysis was conducted using Komodo’s Healthcare Map claims linked with laboratory data of individuals with PBC aged ≥18 years, who started UDCA monotherapy, OCA, or concurrent UDCA/OCA therapy between 09/01/2018 and 09/30/2023 following a 12-month baseline period. Kaplan-Meier estimates assessed treatment persistence after start (index) date of treatment, defined as continuous treatment with an allowable gap of up to 60 days. Logistic regression models estimated the association between a lack of treatment persistence and subsequent ALP normalization (Quest thresholds) assessed between 6-24 months. Pruritus within 24 months post-index, defined with pruritus diagnosis codes and treatments, was compared among treatment groups using logistic regression models. Analyses required 24 months of continuous coverage.
Results: A total of 19,003, 1,903 and 1,581 people with PBC were treated with UDCA, OCA, and concurrent UDCA/OCA, respectively. Study participants’ average age was 62 years, 87% were female and their average Charlson Comorbidity Index was 4.9. At one year, only 42% remained persistent on UDCA, 33% on OCA, and 46% on concurrent OCA/UDCA. In a subgroup of patients (N=2,156) with an ALP test between 6-24 months post index and treated with UDCA, lack of treatment persistence was associated with lower odds of ALP normalization (OR 0.77 [95% CI 0.63-0.93] (Table 1). Pruritus rates in the UDCA, OCA, and OCA/UDCA groups within 24 months were 20.8%, 32.5% (p< .01 relative to UDCA), and 32.1% (p< .01 relative to UDCA), respectively. Compared to UDCA and adjusting for covariates, the OCA and the OCA/UDCA groups had a higher risk of pruritus within 24 months after index (OR 1.54 [95% CI 1.33, 1.79] and 1.55 [1.32, 1.82], respectively).
Discussion: Remaining persistent with UDCA treatment among individuals with PBC should be emphasized, given its potential benefits for ALP normalization. The increased risk of pruritus among patients receiving OCA highlights the need for novel therapies with improved side effect profiles.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kris Kowdley: 89bio – Consultant, Grant/Research Support. AbbVie – Consultant, Grant/Research Support. Boston Pharmaceuticals – Consultant, Grant/Research Support. CymaBay, a Gilead Sciences Company – Consultant, Grant/Research Support. Enanta – Consultant, Grant/Research Support. Genfit – Consultant, Grant/Research Support. Gilead Sciences, Inc. – Consultant, Grant/Research Support. Hanmi – Consultant, Grant/Research Support. HighTide – Consultant, Grant/Research Support. Intercept – Consultant, Grant/Research Support. Ipsen – Consultant, Grant/Research Support. Madrigal – Consultant, Grant/Research Support. NGM – Consultant, Grant/Research Support. Novo Nordisk – Consultant, Grant/Research Support. TERNS – Consultant, Grant/Research Support. Viking – Consultant, Grant/Research Support.
Jonathan Ieyoub: Gilead Sciences – Employee.
Yi Pan: Gilead – Consultant. Stratevi – Employee.
Mihail Samnaliev: Gilead – Consultant. Stratevi – Employee.
Diane Ito: Gilead Sciences – Consultant.
C. Fiorella Murillo Perez: Gilead Sciences – Employee.
Kris V.. Kowdley, MD, FACG1, Jonathan Ieyoub, MS, NP2, Yi Pan, PhD3, Mihail Samnaliev, PhD3, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD2. P4662 - Treatment Persistence and ALP Normalization Among Patients With Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
