Tuesday Poster Session
Category: Liver
P4667 - Cardiovascular Disease Risk and Overall Mortality in Patients With Hepatitis C Infection and Depression: A Large Multicenter Cohort Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Ayowumi A. Adekolu, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Ayowumi A.. Adekolu, MD1, Ethan M. Cohen, MD1, Taylor McCready, MPH2, Olanrewaju Adeniran, MBBS1, Katherine Shepherd, MD1, Joshua Kirkpatrick, MD1, Alejandra Mendez, MD1, Kanith Farah, MD1, Ademola Ajibade, MD1, Samuel Mensa, MBChB1, Carlson Sama, MD1, George Obeng, MD1, Swapna Gayam, MD1
1West Virginia University, Morgantown, WV; 2NYU Grossman School of Medicine, New York, NY
Introduction: Recent studies have shown increased prevalence of major depressive disorder (MDD) in patients with hepatitis C virus (HCV) infection. HCV and MDD have independently been associated with increased risk of cardiovascular disease (CVD) and mortality. However, no studies have assessed CVD risk and mortality in patients with HCV and MDD. This study evaluates the overall mortality and CVD risk in a population with HCV with and without MDD.
Methods: We conducted a population-based, nationwide retrospective cohort study using the TriNetX platform. Adult patients aged ≥18 years old with a diagnosis of HCV were included. In the intervention cohort, participants were included if they had a diagnosis of MDD at least one year after their HCV diagnosis. We excluded patients with chronic liver diseases, cirrhosis, any primary malignancies, and psychoactive substance-related mood disorders. Patients diagnosed with HCV and MDD were matched with patients diagnosed with HCV without MDD using 1:1 propensity score matching (PSM) according to demographics, essential hypertension, type 1 and type 2 diabetes, nicotine dependence, body mass index and history of liver transplant.
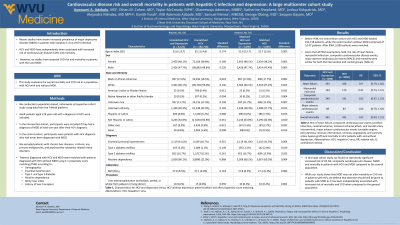
Results: Before PSM, the intervention cohort with HCV and MDD totaled 192,718 patients, while the control cohort without MDD comprised of 5,147 patients. 5,090 patients were matched. Given that all PSM assumptions hold, the risk of heart failure (HF) (RR 0.90; 95% CI 0.79, 1.02), myocardial infarction (MI) (RR 0.91; 95% CI 0.74, 1.12), cerebrovascular disease (RR 1.03; 95% CI 0.87, 1.23), major adverse cardiovascular events (MACE) (RR 1.06; 95% CI 0.79, 1.43) and mortality (RR 1.07; 95% CI 0.94, 1.21) were similar for both the intervention and control groups (Table 1).
Discussion: In this large cohort study, we found no statistically significant increased risk of HF, MI, cerebrovascular disease, MACE and mortality in patients with HCC and MDD compared to the control population. While our study shows that MDD may not alter mortality or CVD risk in patients with HCC, we believe that attention should still be given to patients with MDD as it has been independently associated with increased risk of mortality and CVD when compared to the general population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayowumi A.. Adekolu, MD1, Ethan M. Cohen, MD1, Taylor McCready, MPH2, Olanrewaju Adeniran, MBBS1, Katherine Shepherd, MD1, Joshua Kirkpatrick, MD1, Alejandra Mendez, MD1, Kanith Farah, MD1, Ademola Ajibade, MD1, Samuel Mensa, MBChB1, Carlson Sama, MD1, George Obeng, MD1, Swapna Gayam, MD1. P4667 - Cardiovascular Disease Risk and Overall Mortality in Patients With Hepatitis C Infection and Depression: A Large Multicenter Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2NYU Grossman School of Medicine, New York, NY
Introduction: Recent studies have shown increased prevalence of major depressive disorder (MDD) in patients with hepatitis C virus (HCV) infection. HCV and MDD have independently been associated with increased risk of cardiovascular disease (CVD) and mortality. However, no studies have assessed CVD risk and mortality in patients with HCV and MDD. This study evaluates the overall mortality and CVD risk in a population with HCV with and without MDD.
Methods: We conducted a population-based, nationwide retrospective cohort study using the TriNetX platform. Adult patients aged ≥18 years old with a diagnosis of HCV were included. In the intervention cohort, participants were included if they had a diagnosis of MDD at least one year after their HCV diagnosis. We excluded patients with chronic liver diseases, cirrhosis, any primary malignancies, and psychoactive substance-related mood disorders. Patients diagnosed with HCV and MDD were matched with patients diagnosed with HCV without MDD using 1:1 propensity score matching (PSM) according to demographics, essential hypertension, type 1 and type 2 diabetes, nicotine dependence, body mass index and history of liver transplant.
Results: Before PSM, the intervention cohort with HCV and MDD totaled 192,718 patients, while the control cohort without MDD comprised of 5,147 patients. 5,090 patients were matched. Given that all PSM assumptions hold, the risk of heart failure (HF) (RR 0.90; 95% CI 0.79, 1.02), myocardial infarction (MI) (RR 0.91; 95% CI 0.74, 1.12), cerebrovascular disease (RR 1.03; 95% CI 0.87, 1.23), major adverse cardiovascular events (MACE) (RR 1.06; 95% CI 0.79, 1.43) and mortality (RR 1.07; 95% CI 0.94, 1.21) were similar for both the intervention and control groups (Table 1).
Discussion: In this large cohort study, we found no statistically significant increased risk of HF, MI, cerebrovascular disease, MACE and mortality in patients with HCC and MDD compared to the control population. While our study shows that MDD may not alter mortality or CVD risk in patients with HCC, we believe that attention should still be given to patients with MDD as it has been independently associated with increased risk of mortality and CVD when compared to the general population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayowumi Adekolu indicated no relevant financial relationships.
Ethan Cohen indicated no relevant financial relationships.
Taylor McCready indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Katherine Shepherd indicated no relevant financial relationships.
Joshua Kirkpatrick indicated no relevant financial relationships.
Alejandra Mendez indicated no relevant financial relationships.
Kanith Farah indicated no relevant financial relationships.
Ademola Ajibade indicated no relevant financial relationships.
Samuel Mensa indicated no relevant financial relationships.
Carlson Sama indicated no relevant financial relationships.
George Obeng indicated no relevant financial relationships.
Swapna Gayam indicated no relevant financial relationships.
Ayowumi A.. Adekolu, MD1, Ethan M. Cohen, MD1, Taylor McCready, MPH2, Olanrewaju Adeniran, MBBS1, Katherine Shepherd, MD1, Joshua Kirkpatrick, MD1, Alejandra Mendez, MD1, Kanith Farah, MD1, Ademola Ajibade, MD1, Samuel Mensa, MBChB1, Carlson Sama, MD1, George Obeng, MD1, Swapna Gayam, MD1. P4667 - Cardiovascular Disease Risk and Overall Mortality in Patients With Hepatitis C Infection and Depression: A Large Multicenter Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
