Tuesday Poster Session
Category: Liver
P4700 - Endoscopic Coil and Glue Embolization as an Alternative to Transvenous Obliteration for Salvage Hemostasis of Gastric Varices
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Monica A. Huynh, DO
HCA Florida Largo Hospital
Largo, FL
Presenting Author(s)
Monica A. Huynh Williams, DO1, Alexandra Thomson, MD, MPH2, Jeffrey Kuhary, DO1, Deep Patel, DO1, Vikas Sethi, DO3, Kevin Yeroushalmi, MD1, Roxana Bodin, MD1, Janyll Castineira, DO1, Meir Mizrahi, MD1
1HCA Florida Largo Hospital, Largo, FL; 2Memorial Healthcare System, Savannah, GA; 3HCA Florida Healthcare, Largo, FL
Introduction: Gastroesophageal varices are a potentially life-threatening complication of liver cirrhosis. The current American Association for the Study of Liver Disease guidelines recommend variceal transvenous obliteration (TO) via antegrade or retrograde approach (ATO/RTO) or a transjugular intrahepatic portosystemic shunt (TIPS) in active or for secondary prevention of variceal bleeding.1 Here, we discuss a case of variceal bleeding in a patient who was not a candidate for TO, necessitating endoscopic intervention for salvage hemostasis.
Case Description/Methods: A 33-year-old male with cirrhosis and prior TIPS placement presented for hematemesis requiring mass transfusion protocol. The patient underwent esophagogastroduodenoscopy (EGD) and banding of actively bleeding distal esophageal varices. Imaging revealed extensive thromboses of the TIPS, splenic, right hepatic, main portal, and bilateral portal veins. Attempts at TIPS cannulation by interventional neuroradiology were unsuccessful. The patient was an unsuitable candidate for TO due to the extensive thrombus burden. The patient was transferred to our facility for re-evaluation for TIPS revision versus RTO.
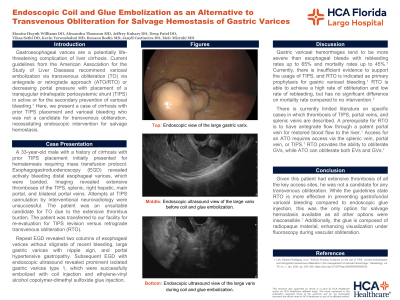
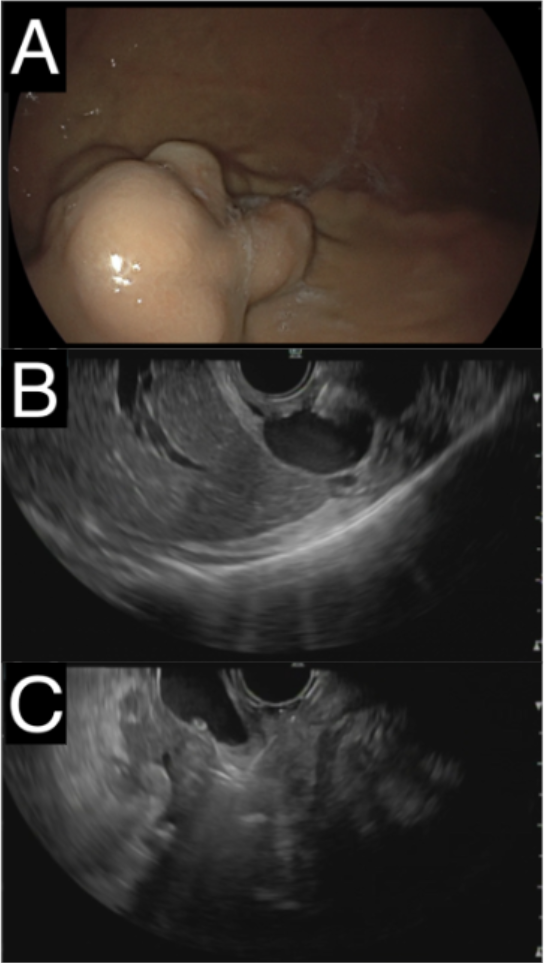
Repeat EGD revealed medium esophageal varices without stigmata of recent bleeding, large gastric varices with nipple sign, and portal hypertensive gastropathy. Endoscopic ultrasound showed prominent isolated gastric varices type 1, which were successfully embolized with coil injection and ethylene-vinyl alcohol copolymer-dimethyl sulfoxide glue injection.
Discussion: Current literature describing cases of concurrent thrombosis of TIPS, portal veins, and splenic veins are limited. Given that this patient had extensive thrombosis of all the key access sites, he was not a candidate for any TO. The guidelines state that RTO is more effective in preventing gastrofundal variceal bleeding compared to endoscopic glue injection, however this was the only option for salvage hemostasis available as all other options were inaccessible. Additionally, the glue is composed of radiopaque material, enhancing visualization under fluoroscopy during vascular obliteration. If rebleeding occurs, this patient would likely require repeat endoscopic intervention with glue injection.
References
Disclosures:
Monica A. Huynh Williams, DO1, Alexandra Thomson, MD, MPH2, Jeffrey Kuhary, DO1, Deep Patel, DO1, Vikas Sethi, DO3, Kevin Yeroushalmi, MD1, Roxana Bodin, MD1, Janyll Castineira, DO1, Meir Mizrahi, MD1. P4700 - Endoscopic Coil and Glue Embolization as an Alternative to Transvenous Obliteration for Salvage Hemostasis of Gastric Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Florida Largo Hospital, Largo, FL; 2Memorial Healthcare System, Savannah, GA; 3HCA Florida Healthcare, Largo, FL
Introduction: Gastroesophageal varices are a potentially life-threatening complication of liver cirrhosis. The current American Association for the Study of Liver Disease guidelines recommend variceal transvenous obliteration (TO) via antegrade or retrograde approach (ATO/RTO) or a transjugular intrahepatic portosystemic shunt (TIPS) in active or for secondary prevention of variceal bleeding.1 Here, we discuss a case of variceal bleeding in a patient who was not a candidate for TO, necessitating endoscopic intervention for salvage hemostasis.
Case Description/Methods: A 33-year-old male with cirrhosis and prior TIPS placement presented for hematemesis requiring mass transfusion protocol. The patient underwent esophagogastroduodenoscopy (EGD) and banding of actively bleeding distal esophageal varices. Imaging revealed extensive thromboses of the TIPS, splenic, right hepatic, main portal, and bilateral portal veins. Attempts at TIPS cannulation by interventional neuroradiology were unsuccessful. The patient was an unsuitable candidate for TO due to the extensive thrombus burden. The patient was transferred to our facility for re-evaluation for TIPS revision versus RTO.
Repeat EGD revealed medium esophageal varices without stigmata of recent bleeding, large gastric varices with nipple sign, and portal hypertensive gastropathy. Endoscopic ultrasound showed prominent isolated gastric varices type 1, which were successfully embolized with coil injection and ethylene-vinyl alcohol copolymer-dimethyl sulfoxide glue injection.
Discussion: Current literature describing cases of concurrent thrombosis of TIPS, portal veins, and splenic veins are limited. Given that this patient had extensive thrombosis of all the key access sites, he was not a candidate for any TO. The guidelines state that RTO is more effective in preventing gastrofundal variceal bleeding compared to endoscopic glue injection, however this was the only option for salvage hemostasis available as all other options were inaccessible. Additionally, the glue is composed of radiopaque material, enhancing visualization under fluoroscopy during vascular obliteration. If rebleeding occurs, this patient would likely require repeat endoscopic intervention with glue injection.
References
Lee, Edward Wolfgang, et al. “AASLD Practice Guidance on the use of TIPS, variceal embolization, and retrograde transvenous obliteration in the management of variceal hemorrhage.” Hepatology, vol. 79, no. 1, Jan. 2024, pp. 224–250, https://doi.org/10.1097/hep.0000000000000530.
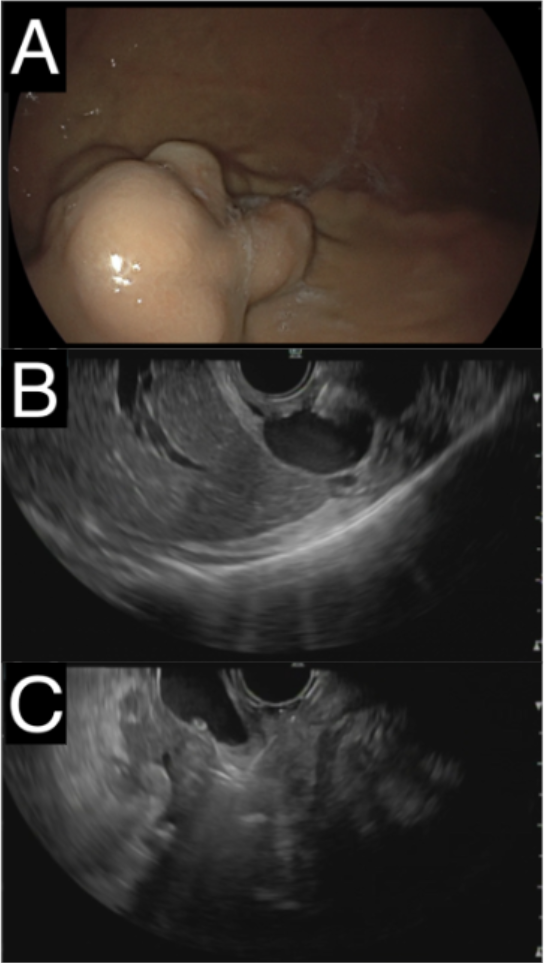
Figure: Figure A: Endoscopic view of the large gastric varix.
Figure B: Endoscopic ultrasound view of the large varix before coil and glue embolization.
Figure C: Endoscopic ultrasound view of the large varix during coil and glue embolization.
Figure B: Endoscopic ultrasound view of the large varix before coil and glue embolization.
Figure C: Endoscopic ultrasound view of the large varix during coil and glue embolization.
Disclosures:
Monica Huynh Williams indicated no relevant financial relationships.
Alexandra Thomson indicated no relevant financial relationships.
Jeffrey Kuhary indicated no relevant financial relationships.
Deep Patel indicated no relevant financial relationships.
Vikas Sethi indicated no relevant financial relationships.
Kevin Yeroushalmi indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Janyll Castineira indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Monica A. Huynh Williams, DO1, Alexandra Thomson, MD, MPH2, Jeffrey Kuhary, DO1, Deep Patel, DO1, Vikas Sethi, DO3, Kevin Yeroushalmi, MD1, Roxana Bodin, MD1, Janyll Castineira, DO1, Meir Mizrahi, MD1. P4700 - Endoscopic Coil and Glue Embolization as an Alternative to Transvenous Obliteration for Salvage Hemostasis of Gastric Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
