Tuesday Poster Session
Category: Liver
P4710 - A Rare Case of Drug-Induced Autoimmune-Like Hepatitis Associated With Labetalol Use
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Laura Miranda, MD
Broward Health North
Pompano Beach, FL
Presenting Author(s)
Laura Miranda, MD1, Anjo Chacko, MD2, Gautam Anand, MD3, John Rivas, MD4
1Broward Health North, Pompano Beach, FL; 2Broward Health North, Deerfield Beach, FL; 3Broward Health North, Fort Lauderdale, FL; 4Broward Health, Hollywood, FL
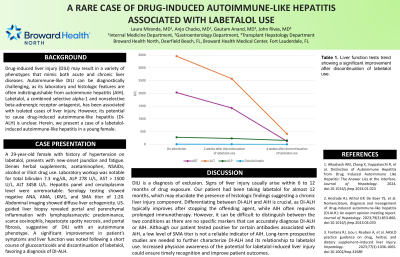
Introduction: Drug-induced liver injury (DILI) may result in a variety of phenotypes that mimic both acute and chronic liver diseases. Autoimmune-like DILI can be diagnostically challenging, as its laboratory and histologic features are often indistinguishable from autoimmune hepatitis (AIH). Labetalol, a combined selective alpha-1 and nonselective beta-adrenergic receptor antagonist, has been associated with isolated cases of liver injury. However, its potential to cause drug-induced autoimmune-like hepatitis (DI-ALH) is unclear. Herein, we present a case of a labetalol-induced autoimmune-like hepatitis in a young female.
Case Description/Methods: A 29-year-old female with history of hypertension on labetalol, presents with new-onset jaundice and fatigue. Denies herbal supplements, acetaminophen, NSAIDs, alcohol or illicit drug use. Laboratory workup was notable for total bilirubin 7.3 mg/dL, ALP 278 U/L, AST > 1500 U/L, ALT 3458 U/L. Hepatitis panel and ceruloplasmin level were unremarkable. Serology testing showed negative ANA, AMA, LKM1, and SMA titer of 1:20. Abdominal imaging showed diffuse liver echogenicity. US-guided liver biopsy revealed portal and parenchymal inflammation with lymphoplasmacytic predominance, scarce eosinophils, hepatocyte spotty necrosis, and portal fibrosis, suggestive of DILI with an autoimmune phenotype. A significant improvement in patient’s symptoms and liver function was noted following a short course of glucocorticoids and discontinuation of labetalol, favoring a diagnosis of DI-ALH.
Discussion: DILI is a diagnosis of exclusion. Signs of liver injury usually arise within 6 to 12 months of drug exposure. Our patient had been taking labetalol for almost 12 months, which may elucidate the presence of histologic findings suggesting a chronic liver injury component. Differentiating between DI-ALH and AIH is crucial, as DI-ALH typically improves after stopping the offending agent, while AIH often requires prolonged immunotherapy. However, it can be difficult to distinguish between the two conditions as there are no specific markers that can accurately diagnose DI-ALH or AIH. Although our patient tested positive for certain antibodies associated with AIH, a low level of SMA titer is not a reliable indicator of AIH. Long-term prospective studies are needed to further characterize DI-ALH and its relationship to labetalol use. Increased physician awareness of the potential for labetalol-induced liver injury could ensure timely recognition and improve patient outcomes.
Disclosures:
Laura Miranda, MD1, Anjo Chacko, MD2, Gautam Anand, MD3, John Rivas, MD4. P4710 - A Rare Case of Drug-Induced Autoimmune-Like Hepatitis Associated With Labetalol Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Broward Health North, Pompano Beach, FL; 2Broward Health North, Deerfield Beach, FL; 3Broward Health North, Fort Lauderdale, FL; 4Broward Health, Hollywood, FL
Introduction: Drug-induced liver injury (DILI) may result in a variety of phenotypes that mimic both acute and chronic liver diseases. Autoimmune-like DILI can be diagnostically challenging, as its laboratory and histologic features are often indistinguishable from autoimmune hepatitis (AIH). Labetalol, a combined selective alpha-1 and nonselective beta-adrenergic receptor antagonist, has been associated with isolated cases of liver injury. However, its potential to cause drug-induced autoimmune-like hepatitis (DI-ALH) is unclear. Herein, we present a case of a labetalol-induced autoimmune-like hepatitis in a young female.
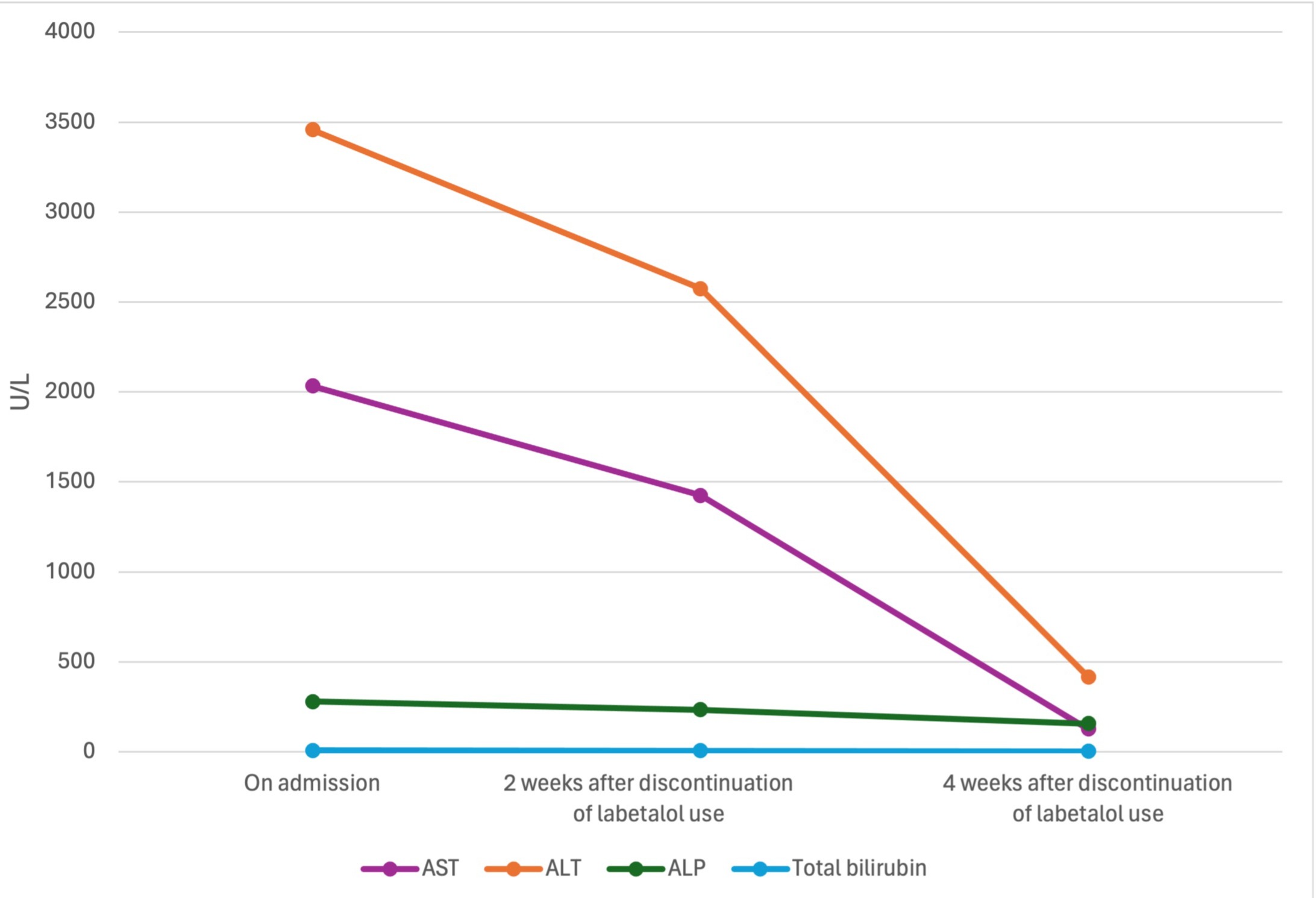
Case Description/Methods: A 29-year-old female with history of hypertension on labetalol, presents with new-onset jaundice and fatigue. Denies herbal supplements, acetaminophen, NSAIDs, alcohol or illicit drug use. Laboratory workup was notable for total bilirubin 7.3 mg/dL, ALP 278 U/L, AST > 1500 U/L, ALT 3458 U/L. Hepatitis panel and ceruloplasmin level were unremarkable. Serology testing showed negative ANA, AMA, LKM1, and SMA titer of 1:20. Abdominal imaging showed diffuse liver echogenicity. US-guided liver biopsy revealed portal and parenchymal inflammation with lymphoplasmacytic predominance, scarce eosinophils, hepatocyte spotty necrosis, and portal fibrosis, suggestive of DILI with an autoimmune phenotype. A significant improvement in patient’s symptoms and liver function was noted following a short course of glucocorticoids and discontinuation of labetalol, favoring a diagnosis of DI-ALH.
Discussion: DILI is a diagnosis of exclusion. Signs of liver injury usually arise within 6 to 12 months of drug exposure. Our patient had been taking labetalol for almost 12 months, which may elucidate the presence of histologic findings suggesting a chronic liver injury component. Differentiating between DI-ALH and AIH is crucial, as DI-ALH typically improves after stopping the offending agent, while AIH often requires prolonged immunotherapy. However, it can be difficult to distinguish between the two conditions as there are no specific markers that can accurately diagnose DI-ALH or AIH. Although our patient tested positive for certain antibodies associated with AIH, a low level of SMA titer is not a reliable indicator of AIH. Long-term prospective studies are needed to further characterize DI-ALH and its relationship to labetalol use. Increased physician awareness of the potential for labetalol-induced liver injury could ensure timely recognition and improve patient outcomes.
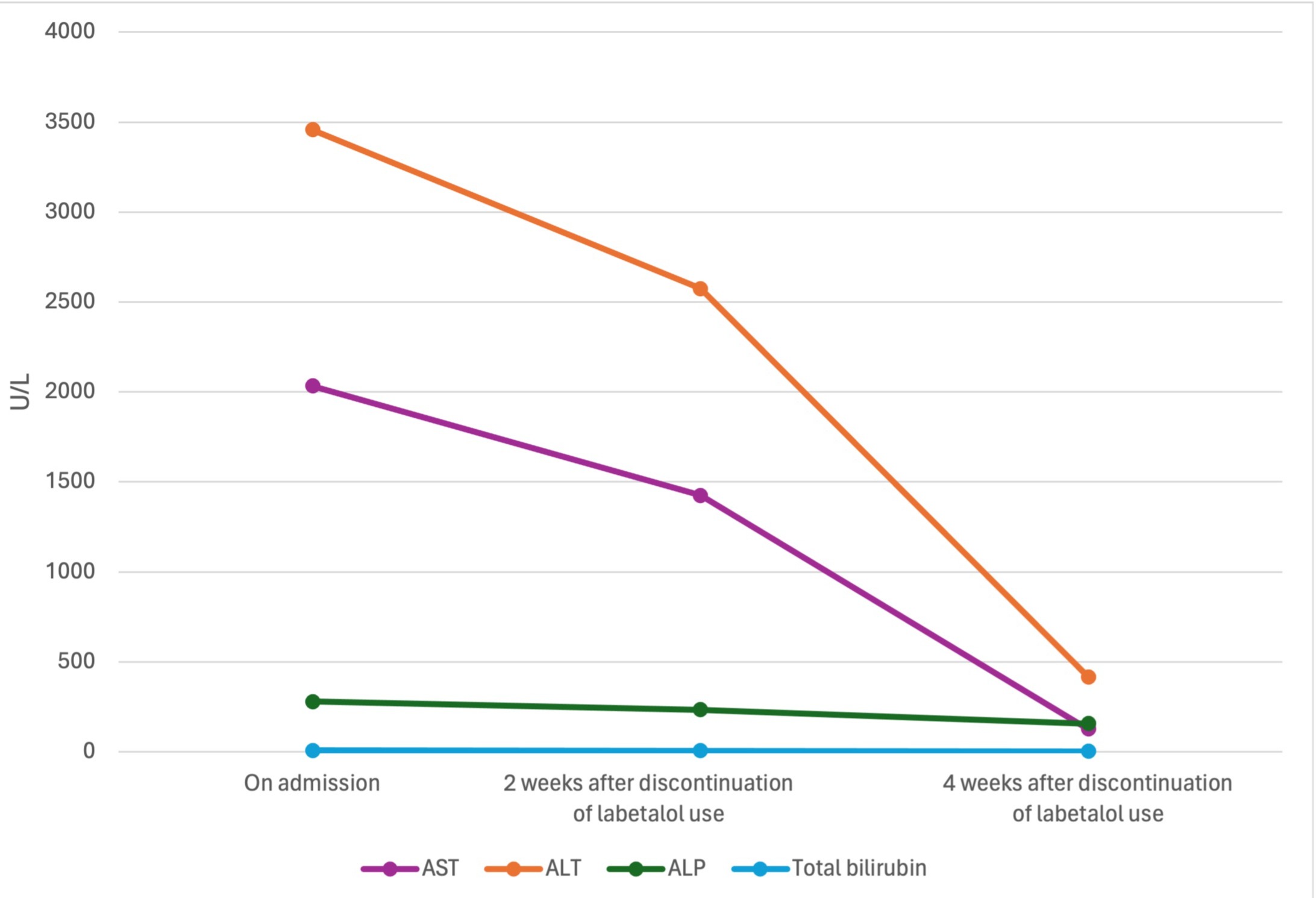
Figure: Liver function tests trend showing a significant improvement after discontinuation of labetalol use.
Disclosures:
Laura Miranda indicated no relevant financial relationships.
Anjo Chacko indicated no relevant financial relationships.
Gautam Anand indicated no relevant financial relationships.
John Rivas indicated no relevant financial relationships.
Laura Miranda, MD1, Anjo Chacko, MD2, Gautam Anand, MD3, John Rivas, MD4. P4710 - A Rare Case of Drug-Induced Autoimmune-Like Hepatitis Associated With Labetalol Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
