Tuesday Poster Session
Category: Liver
P4713 - A Post-Transplant Immunosuppression Complication: EBV-Positive Classic Hodgkin Lymphoma PTLD Mimicking as Cholangiocarcinoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Himesh Zaver, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Himesh Zaver, MD, Jason Erno, MD, Gautham Prakash, MD, Samuel Plant, MD, Jigisha Chaudhari, MD, Ayman Mithqal, MD, Elizabeth Courville, MD, Enrica Marchi, MD, Zachary Henry, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a life-threatening complication after solid organ transplantation. We present a case of Epstein-Barr virus (EBV)-positive classic Hodgkin lymphoma (cHL) PTLD after liver transplantation originally concerning for a solitary liver mass.
Case Description/Methods: A 65-year-old, male patient presented to a tertiary care liver transplant center endorsing a 6 week history of fatigue, jaundice, and right upper quadrant pain. The patient underwent deceased donor, orthotopic liver transplantation eighteen months prior for fulminant autoimmune hepatitis. One month prior to his current presentation the patient endorsed disruption in his immunosuppression regimen prompting an empiric increase in his immunosuppression regimen by his local hepatologist.
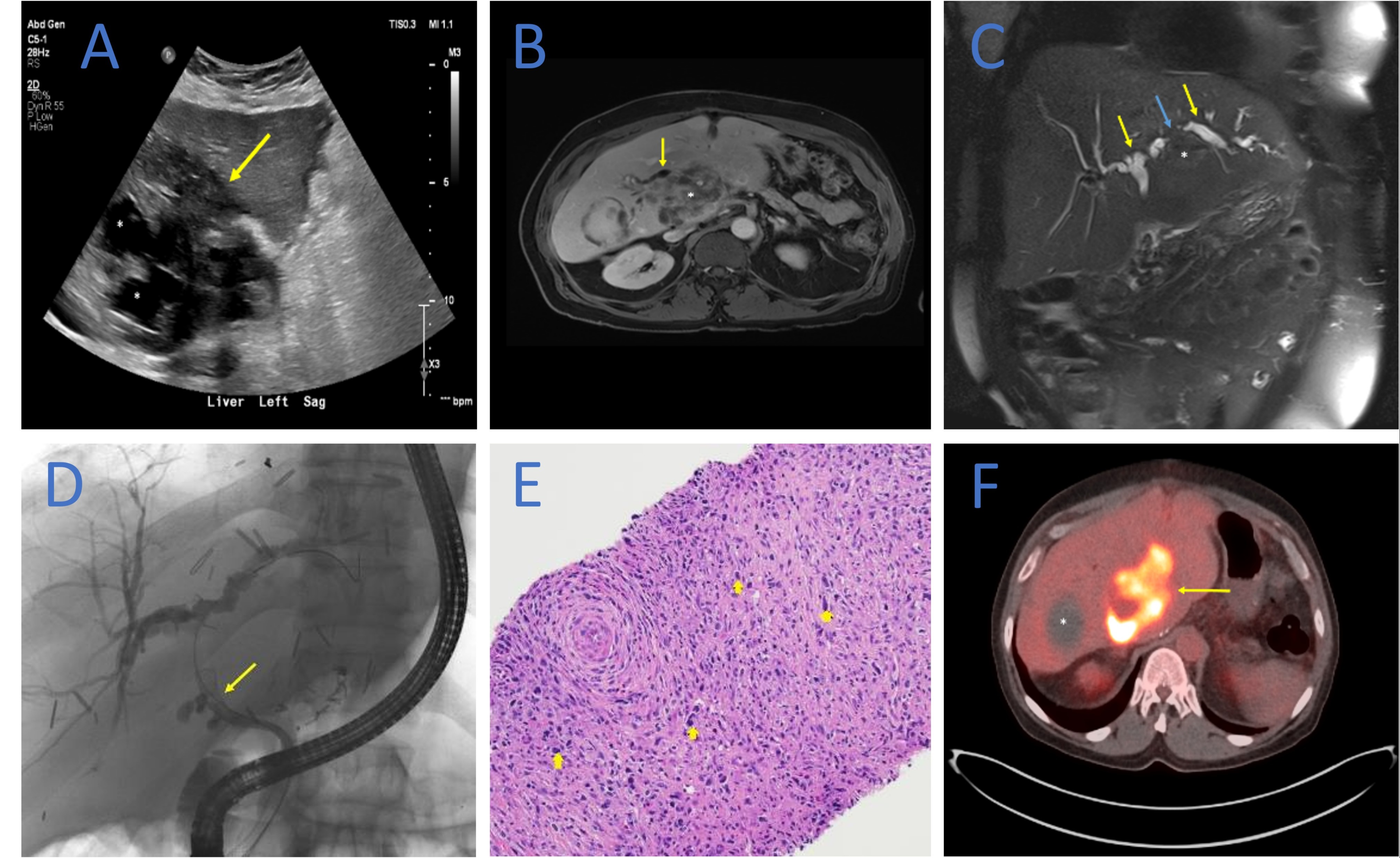
Workup on hospital admission was supportive of a positive EBV viral load and elevated liver enzymes, bilirubin, and Carbohydrate antigen 19-9 (Table 1). A liver ultrasound was significant for an ill-defined mass (Figure A). Magnetic resonance imaging of his abdomen further characterized a seven centimeter mass involving the caudate lobe and a possible post-transplant, anastomotic biliary stricture (Figure B,C).
Following balloon dilation of the stricture, one fully covered metal stent was successfully placed into the common hepatic duct via ERCP (Figure D). Brush cytology from the bile duct stricture was negative for malignancy. Ultrasound guided biopsy of the liver mass was supportive of cHL consistent with EBV-associated cHL-PTLD (Figure E). Positron emission tomography test for treatment planning was supportive of stage IE bulky cHL (Figure F).
To induce remission of EBV viremia, a dose reduction of the patient’s immunosuppression regimen to a minimum level necessary to prevent graft rejection was used. The patient received Rituximab and then started an anthracycline-based chemotherapy regimen for cHL-PTLD thereafter. Following ERCP and initiation of chemotherapy treatment the patient's symptoms resolved and abnormal labs normalized.
Discussion: PTLD occurs in about 1-2% of adult liver transplants. Most cases are due to reactivation of latent EBV during post-transplant management with immunosuppressive medications. Reduction of immunosuppression and restoration of a functional immune system is one of the most important aspects of PTLD management. However, this must be balanced with the risk of transplant rejection.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Himesh Zaver, MD, Jason Erno, MD, Gautham Prakash, MD, Samuel Plant, MD, Jigisha Chaudhari, MD, Ayman Mithqal, MD, Elizabeth Courville, MD, Enrica Marchi, MD, Zachary Henry, MD. P4713 - A Post-Transplant Immunosuppression Complication: EBV-Positive Classic Hodgkin Lymphoma PTLD Mimicking as Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a life-threatening complication after solid organ transplantation. We present a case of Epstein-Barr virus (EBV)-positive classic Hodgkin lymphoma (cHL) PTLD after liver transplantation originally concerning for a solitary liver mass.
Case Description/Methods: A 65-year-old, male patient presented to a tertiary care liver transplant center endorsing a 6 week history of fatigue, jaundice, and right upper quadrant pain. The patient underwent deceased donor, orthotopic liver transplantation eighteen months prior for fulminant autoimmune hepatitis. One month prior to his current presentation the patient endorsed disruption in his immunosuppression regimen prompting an empiric increase in his immunosuppression regimen by his local hepatologist.
Workup on hospital admission was supportive of a positive EBV viral load and elevated liver enzymes, bilirubin, and Carbohydrate antigen 19-9 (Table 1). A liver ultrasound was significant for an ill-defined mass (Figure A). Magnetic resonance imaging of his abdomen further characterized a seven centimeter mass involving the caudate lobe and a possible post-transplant, anastomotic biliary stricture (Figure B,C).
Following balloon dilation of the stricture, one fully covered metal stent was successfully placed into the common hepatic duct via ERCP (Figure D). Brush cytology from the bile duct stricture was negative for malignancy. Ultrasound guided biopsy of the liver mass was supportive of cHL consistent with EBV-associated cHL-PTLD (Figure E). Positron emission tomography test for treatment planning was supportive of stage IE bulky cHL (Figure F).
To induce remission of EBV viremia, a dose reduction of the patient’s immunosuppression regimen to a minimum level necessary to prevent graft rejection was used. The patient received Rituximab and then started an anthracycline-based chemotherapy regimen for cHL-PTLD thereafter. Following ERCP and initiation of chemotherapy treatment the patient's symptoms resolved and abnormal labs normalized.
Discussion: PTLD occurs in about 1-2% of adult liver transplants. Most cases are due to reactivation of latent EBV during post-transplant management with immunosuppressive medications. Reduction of immunosuppression and restoration of a functional immune system is one of the most important aspects of PTLD management. However, this must be balanced with the risk of transplant rejection.
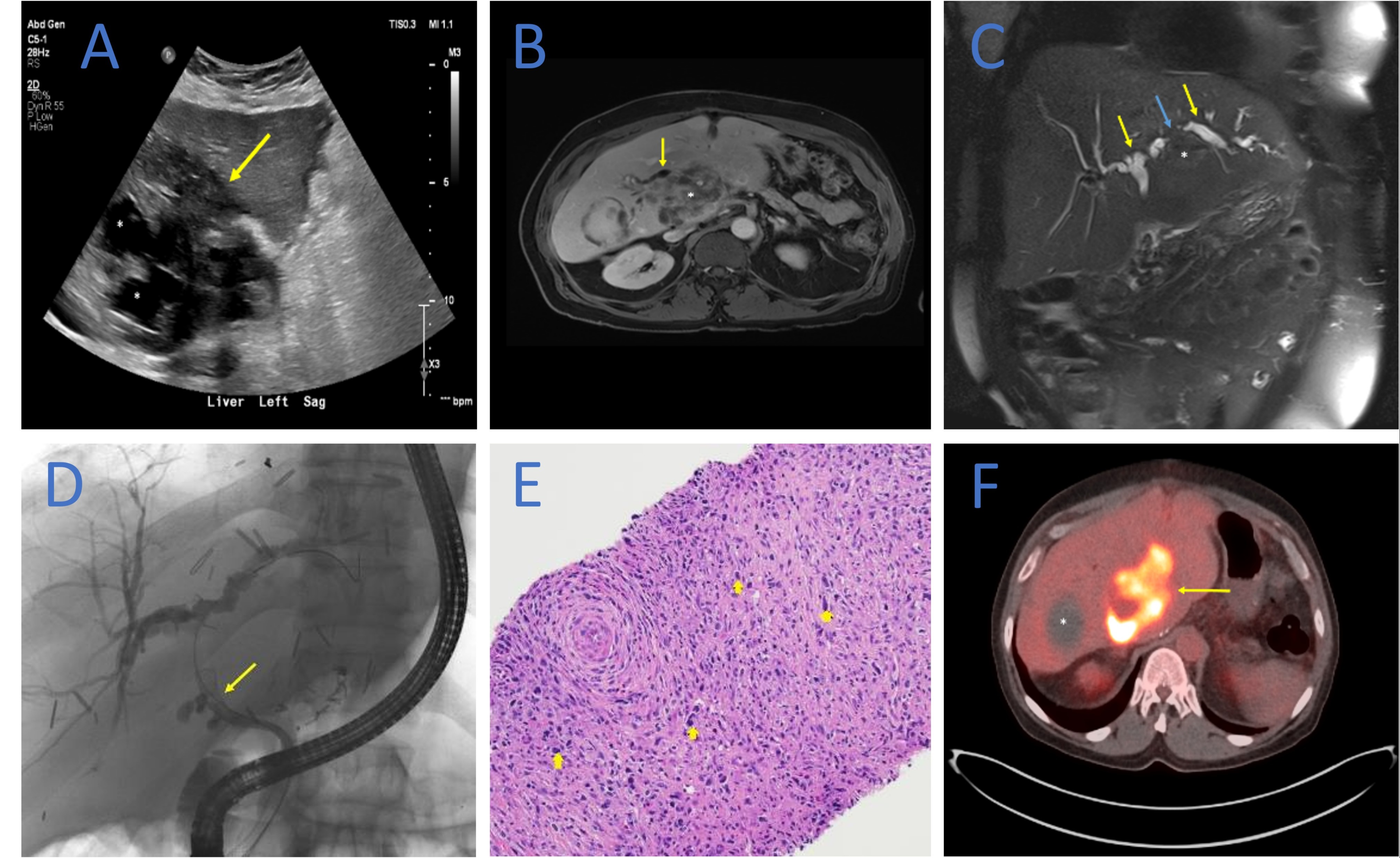
Figure: Figure A-F; Cross sectional imaging and pathology supporting Epstein-Barr virus (EBV)-positive, classic Hodgkin lymphoma (cHL) Post-transplant lymphoproliferative disorder (PTLD)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Himesh Zaver indicated no relevant financial relationships.
Jason Erno indicated no relevant financial relationships.
Gautham Prakash indicated no relevant financial relationships.
Samuel Plant indicated no relevant financial relationships.
Jigisha Chaudhari indicated no relevant financial relationships.
Ayman Mithqal indicated no relevant financial relationships.
Elizabeth Courville indicated no relevant financial relationships.
Enrica Marchi indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Himesh Zaver, MD, Jason Erno, MD, Gautham Prakash, MD, Samuel Plant, MD, Jigisha Chaudhari, MD, Ayman Mithqal, MD, Elizabeth Courville, MD, Enrica Marchi, MD, Zachary Henry, MD. P4713 - A Post-Transplant Immunosuppression Complication: EBV-Positive Classic Hodgkin Lymphoma PTLD Mimicking as Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

