Tuesday Poster Session
Category: Liver
P4715 - The Dark Side of Slimming: Weight Loss Supplement Induced Liver Injury
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Spandana Alluri, MS, MD
Henry Ford Health
West Bloomfield, MI
Presenting Author(s)
Spandana Alluri, MS, MD1, John Lloyd, BS2, Allyce N. Caines, MD3
1Henry Ford Health, West Bloomfield, MI; 2Wayne State University, Detroit, MI; 3Henry Ford Health, Detroit, MI
Introduction: Drug-induced liver injury (DILI) is a significant and underrecognized cause of acute liver failure, with weight loss supplements being a notable culprit due to unregulated ingredients and widespread use. Diversity of causative agents in DILI results in a sundry of clinical presentations that often mimic other liver diseases, making diagnosis complex. This case report delves into the diagnostic challenges and clinical implications of DILI.
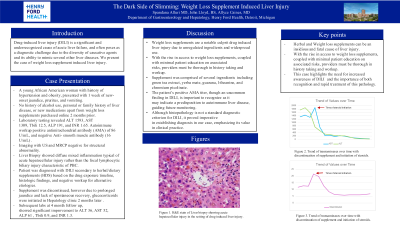
Case Description/Methods: A young African American woman with history of hypertension and obesity, presented with 1 week of new-onset jaundice, pruritus, and vomiting. She denied alcohol use, personal or family history of liver disease, or new medications apart from weight loss supplements purchased online 2 months prior. Initial lab work revealed ALT 1593, AST 1309, Tbili 12.5, ALP 191, and INR 1.65. Infectious, metabolic workup was negative, with positive antimitochondrial antibody (AMA) of 86 U/mL, and negative Anti- smooth muscle antibody (16 U/mL) . Subsequent imaging with US and MRCP showed no structural abnormality. Liver biopsy done to differentiate drug induced liver injury (DILI), drug induced autoimmune liver disease, and autoimmune related liver disease and/or overlap syndrome. Biopsy showed diffuse mixed inflammation typical of acute hepatocellular injury rather than the focal lymphocytic biliary injury characteristic of PBC. Patient was diagnosed with DILI secondary to herbal/dietary supplements (HDS) based on the drug exposure timeline, histologic findings, and the negative workup for alternative etiologies. Supplement was discontinued, however due to prolonged jaundice and lack of spontaneous recovery, glucocorticoids were initiated in Hepatology clinic 2 months later . Subsequent labs at 4 month follow up, showed significant improvement to ALT 36, AST 52, ALP 61 , Tbili 0.9, and INR 1.3.
Discussion: This case highlights the need for awareness of DILI, which is often underreported and can lead to severe outcomes. With the rise in access to weight loss supplements, coupled with minimal patient education on associated risks, providers must be thorough in history taking and workup. The patient’s positive AMA titer, though an uncommon finding in DILI, is important to recognize as it may indicate a predisposition to autoimmune liver disease, guiding future monitoring. Although histopathology is not a standard diagnostic criterion for DILI, it proved imperative in establishing diagnosis in our case, emphasizing its value in clinical practice.
Disclosures:
Spandana Alluri, MS, MD1, John Lloyd, BS2, Allyce N. Caines, MD3. P4715 - The Dark Side of Slimming: Weight Loss Supplement Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, West Bloomfield, MI; 2Wayne State University, Detroit, MI; 3Henry Ford Health, Detroit, MI
Introduction: Drug-induced liver injury (DILI) is a significant and underrecognized cause of acute liver failure, with weight loss supplements being a notable culprit due to unregulated ingredients and widespread use. Diversity of causative agents in DILI results in a sundry of clinical presentations that often mimic other liver diseases, making diagnosis complex. This case report delves into the diagnostic challenges and clinical implications of DILI.
Case Description/Methods: A young African American woman with history of hypertension and obesity, presented with 1 week of new-onset jaundice, pruritus, and vomiting. She denied alcohol use, personal or family history of liver disease, or new medications apart from weight loss supplements purchased online 2 months prior. Initial lab work revealed ALT 1593, AST 1309, Tbili 12.5, ALP 191, and INR 1.65. Infectious, metabolic workup was negative, with positive antimitochondrial antibody (AMA) of 86 U/mL, and negative Anti- smooth muscle antibody (16 U/mL) . Subsequent imaging with US and MRCP showed no structural abnormality. Liver biopsy done to differentiate drug induced liver injury (DILI), drug induced autoimmune liver disease, and autoimmune related liver disease and/or overlap syndrome. Biopsy showed diffuse mixed inflammation typical of acute hepatocellular injury rather than the focal lymphocytic biliary injury characteristic of PBC. Patient was diagnosed with DILI secondary to herbal/dietary supplements (HDS) based on the drug exposure timeline, histologic findings, and the negative workup for alternative etiologies. Supplement was discontinued, however due to prolonged jaundice and lack of spontaneous recovery, glucocorticoids were initiated in Hepatology clinic 2 months later . Subsequent labs at 4 month follow up, showed significant improvement to ALT 36, AST 52, ALP 61 , Tbili 0.9, and INR 1.3.
Discussion: This case highlights the need for awareness of DILI, which is often underreported and can lead to severe outcomes. With the rise in access to weight loss supplements, coupled with minimal patient education on associated risks, providers must be thorough in history taking and workup. The patient’s positive AMA titer, though an uncommon finding in DILI, is important to recognize as it may indicate a predisposition to autoimmune liver disease, guiding future monitoring. Although histopathology is not a standard diagnostic criterion for DILI, it proved imperative in establishing diagnosis in our case, emphasizing its value in clinical practice.
Disclosures:
Spandana Alluri indicated no relevant financial relationships.
John Lloyd indicated no relevant financial relationships.
Allyce Caines indicated no relevant financial relationships.
Spandana Alluri, MS, MD1, John Lloyd, BS2, Allyce N. Caines, MD3. P4715 - The Dark Side of Slimming: Weight Loss Supplement Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
