Tuesday Poster Session
Category: Liver
P4718 - Idiopathic Refractory Ascites: A Rare and Fatal Complication of Haemopoietic Stem Cell Transplant in a Patient With Acute Myelogenous Leukemia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JK
Jeffrey Kwan, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Jeffrey Kwan, MD1, Robert Spiller, DO, MS2, Lukman Cheraghvandi, MD3, Arul M. Thomas, MD4
1Walter Reed National Military Medical Center, Bethesda, MD; 2Walter Reed National Military Medical Center, Silver Spring, MD; 3MedStar Georgetown University Hospital, Washington, DC; 4Medstar Georgetown University Hospital, Washington, DC
Introduction: Haemopoietic stem cell transplant (HSCT) is a life-saving treatment utilized in many hematological malignancies. Hepatic complications of HSCT can present a diagnostic challenge in immunocompromised patients and idiopathic refractory ascites (IRA) is a rare complication.
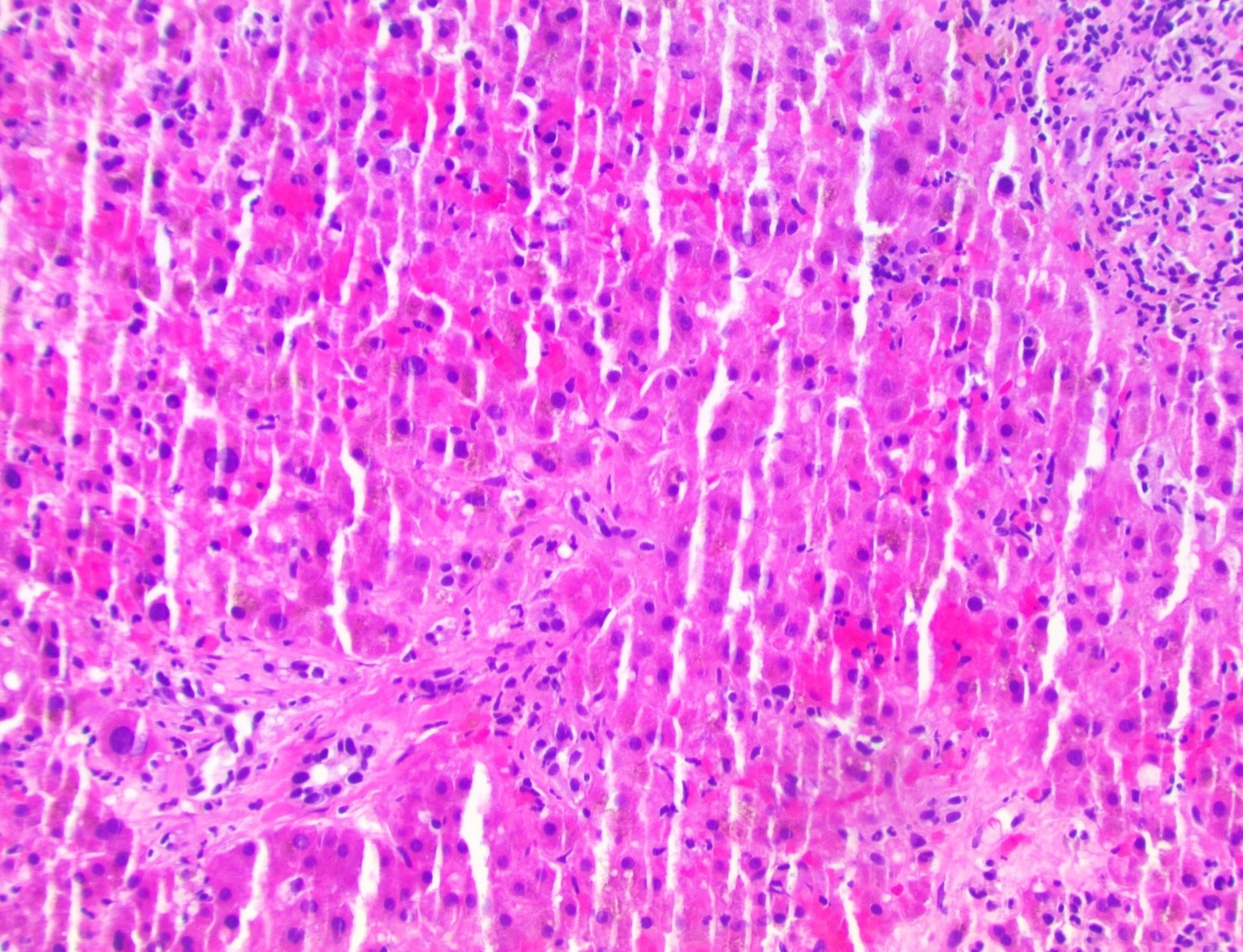
Case Description/Methods: A 65-year-old male with acute myelogenous leukemia status post HSCT developed chronic graft versus host disease (cGVHD) with mucocutaneous disease nine months after transplant and was treated with ruxolitinib. Three months later, he was admitted for sepsis due to bacteremia and noted to have new onset ascites without a history of liver disease. Echocardiogram, ultrasound of liver vasculature and GFR were normal. Workup for secondary causes was negative (table 1) and transjugular liver biopsy showed stage 2 fibrosis and no features of sinusoidal obstruction syndrome (SOS) (figure 1). During evaluation of recurrent aspiration pneumonia, CT incidentally showed large esophageal varices. During EGD, the scope was unable to pass the proximal esophagus, likely due to an esophageal web; a defining diagnostic criterion for GI involvement of cGVHD. Abatacept and methylprednisolone were started due to persistently elevated liver enzymes and worsening of GVHD. IRA was considered due to elevated serum ascites albumin gradient ( >1.1), elevated hepatic venous pressure gradient (32mmHg), no evidence of SOS and no alternative etiology for portal hypertension. Treatment of IRA with defibrotide was considered but he succumbed to recurrent aspiration pneumonia.
Discussion: Non-cirrhotic portal hypertension presents a challenging differential in the post-HSCT patient. HGVHD must be considered and aggressively treated as the 1-year mortality is 68%. Consideration of ruxolitinib for steroid-refractory GVHD provides an overall response rate of 86.9%, but the hepatic specific response is only 26-53%. Without other organ involvement, liver biopsy is performed to rule out SOS as it presents similarly to hGVHD but has an equally high mortality rate of >80% but is managed with defibrotide. Without a pathologic diagnosis of SOS, IRA should be considered given its similar mortality rate of 63%. IRA after HSCT is a rare and fatal disease process that is poorly understood with no consensus on treatment. To date, literature review shows only one successful treatment of IRA with ibrutinib, which requires further research. Clinicians should be aware of IRA when working up post-HSCT patients with new ascites.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jeffrey Kwan, MD1, Robert Spiller, DO, MS2, Lukman Cheraghvandi, MD3, Arul M. Thomas, MD4. P4718 - Idiopathic Refractory Ascites: A Rare and Fatal Complication of Haemopoietic Stem Cell Transplant in a Patient With Acute Myelogenous Leukemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2Walter Reed National Military Medical Center, Silver Spring, MD; 3MedStar Georgetown University Hospital, Washington, DC; 4Medstar Georgetown University Hospital, Washington, DC
Introduction: Haemopoietic stem cell transplant (HSCT) is a life-saving treatment utilized in many hematological malignancies. Hepatic complications of HSCT can present a diagnostic challenge in immunocompromised patients and idiopathic refractory ascites (IRA) is a rare complication.
Case Description/Methods: A 65-year-old male with acute myelogenous leukemia status post HSCT developed chronic graft versus host disease (cGVHD) with mucocutaneous disease nine months after transplant and was treated with ruxolitinib. Three months later, he was admitted for sepsis due to bacteremia and noted to have new onset ascites without a history of liver disease. Echocardiogram, ultrasound of liver vasculature and GFR were normal. Workup for secondary causes was negative (table 1) and transjugular liver biopsy showed stage 2 fibrosis and no features of sinusoidal obstruction syndrome (SOS) (figure 1). During evaluation of recurrent aspiration pneumonia, CT incidentally showed large esophageal varices. During EGD, the scope was unable to pass the proximal esophagus, likely due to an esophageal web; a defining diagnostic criterion for GI involvement of cGVHD. Abatacept and methylprednisolone were started due to persistently elevated liver enzymes and worsening of GVHD. IRA was considered due to elevated serum ascites albumin gradient ( >1.1), elevated hepatic venous pressure gradient (32mmHg), no evidence of SOS and no alternative etiology for portal hypertension. Treatment of IRA with defibrotide was considered but he succumbed to recurrent aspiration pneumonia.
Discussion: Non-cirrhotic portal hypertension presents a challenging differential in the post-HSCT patient. HGVHD must be considered and aggressively treated as the 1-year mortality is 68%. Consideration of ruxolitinib for steroid-refractory GVHD provides an overall response rate of 86.9%, but the hepatic specific response is only 26-53%. Without other organ involvement, liver biopsy is performed to rule out SOS as it presents similarly to hGVHD but has an equally high mortality rate of >80% but is managed with defibrotide. Without a pathologic diagnosis of SOS, IRA should be considered given its similar mortality rate of 63%. IRA after HSCT is a rare and fatal disease process that is poorly understood with no consensus on treatment. To date, literature review shows only one successful treatment of IRA with ibrutinib, which requires further research. Clinicians should be aware of IRA when working up post-HSCT patients with new ascites.
Figure: Hepatic lobules show patchy zonal coagulative necrosis, lobular predominant lymphoplasmacytic hepatitis. Portal tracts show patchy triaditis with neutrophilic/lymphocytic infiltrate with no frank ductilitis or ductular atrophy or apoptosis. 20x micrograph, H&E stain.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jeffrey Kwan indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
Lukman Cheraghvandi indicated no relevant financial relationships.
Arul M. Thomas indicated no relevant financial relationships.
Jeffrey Kwan, MD1, Robert Spiller, DO, MS2, Lukman Cheraghvandi, MD3, Arul M. Thomas, MD4. P4718 - Idiopathic Refractory Ascites: A Rare and Fatal Complication of Haemopoietic Stem Cell Transplant in a Patient With Acute Myelogenous Leukemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
