Tuesday Poster Session
Category: Liver
P4731 - Simultaneous Presentation of Post-Transplant Lymphoproliferative Disorder (PTLD) and Acute Cellular Rejection (ACR) in a Liver Transplant Recipient: A Therapeutic Conundrum
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ankit Mishra, MD
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Ankit Mishra, MD1, Priya Kathuria, MD1, Dhiraj Peddu, MD2, Matthew Kubina, MD1, Hellan Kwon, MD2, Shannon Carty, MD2, Patricia Bloom, MD2
1University of Michigan, Ann Arbor, MI; 2University of Michigan Health, Ann Arbor, MI
Introduction: Post-transplant lymphoproliferative disorder (PTLD) and severe acute cellular rejection (SACR) are post liver transplant complications, each requiring distinct treatment strategies. First-line treatment for PTLD, a malignancy related to immunosuppression (IS), is reduction in IS, while ACR is typically managed by increasing IS. This case highlights the challenge of managing both PTLD and severe ACR.
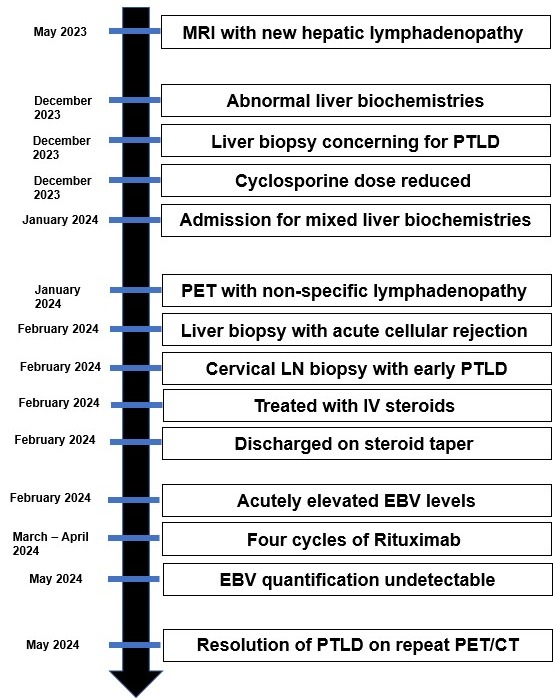
Case Description/Methods: A 64-year-old man with a history of cirrhosis, and hepatocellular carcinoma underwent orthotopic liver transplant (D EBV+, R EBV -) in August 2022. A liver MRI in May 2023 revealed new porta-hepatic lymphadenopathy. Subsequently, two negative endoscopic ultrasound guided biopsies were performed. A follow-up MRI in November 2023 showed continued enlarging lymph nodes. In December of 2023 elevated cholestatic liver biochemistries led to a liver biopsy, which showed few aggregates of small lymphocytes and scattered EBV+ cells, with a quantitative EBV (qEBV) level of 42,882 IU/mL. Due to concerns for PTLD, his cyclosporine dose was reduced from 100 mg to 75 mg twice daily. In January of 2024, the patient was admitted for liver biochemistries consistent with mixed pattern of injury in the setting of recently decreased IS (AST 93321, ALT 117 420, ALP 187287, and Total bilirubin 0.8 1.1).
A PET scan during admission showed non-specific lymphadenopathy in the thorax, abdomen, and pelvis, with a qEBV level of 2,518 IU/mL. Biopsies of a cervical lymph node and liver were performed. The liver biopsy indicated severe bile duct injury, and endotheliitis suggesting SACR. The cervical lymph node biopsy showed follicular hyperplasia with numerous EBV+ cells, consistent with early/non-destructive PTLD. After discussion with multiple specialists the patient was treated with three days of high-dose steroids for SACR. Shortly after IV steroid treatment, he was discharged with a steroid taper and his home IS regimen. Outpatient lab tests showed improved liver biochemistries but an acutely elevated EBV level to 10,252 IU/mL, concerning for rapidly progressing PTLD. He was seen by hematology and received four cycles of Rituximab for PTLD. Post-treatment, his EBV quantification was undetectable, and PET/CT demonstrated complete metabolic response.
Discussion: Our case illustrates the clinical conundrum where increased and decreased IS are simultaneously indicated, requiring individualized therapy. The use of high-dose steroids followed by Rituximab effectively managed both conditions.
Disclosures:
Ankit Mishra, MD1, Priya Kathuria, MD1, Dhiraj Peddu, MD2, Matthew Kubina, MD1, Hellan Kwon, MD2, Shannon Carty, MD2, Patricia Bloom, MD2. P4731 - Simultaneous Presentation of Post-Transplant Lymphoproliferative Disorder (PTLD) and Acute Cellular Rejection (ACR) in a Liver Transplant Recipient: A Therapeutic Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2University of Michigan Health, Ann Arbor, MI
Introduction: Post-transplant lymphoproliferative disorder (PTLD) and severe acute cellular rejection (SACR) are post liver transplant complications, each requiring distinct treatment strategies. First-line treatment for PTLD, a malignancy related to immunosuppression (IS), is reduction in IS, while ACR is typically managed by increasing IS. This case highlights the challenge of managing both PTLD and severe ACR.
Case Description/Methods: A 64-year-old man with a history of cirrhosis, and hepatocellular carcinoma underwent orthotopic liver transplant (D EBV+, R EBV -) in August 2022. A liver MRI in May 2023 revealed new porta-hepatic lymphadenopathy. Subsequently, two negative endoscopic ultrasound guided biopsies were performed. A follow-up MRI in November 2023 showed continued enlarging lymph nodes. In December of 2023 elevated cholestatic liver biochemistries led to a liver biopsy, which showed few aggregates of small lymphocytes and scattered EBV+ cells, with a quantitative EBV (qEBV) level of 42,882 IU/mL. Due to concerns for PTLD, his cyclosporine dose was reduced from 100 mg to 75 mg twice daily. In January of 2024, the patient was admitted for liver biochemistries consistent with mixed pattern of injury in the setting of recently decreased IS (AST 93321, ALT 117 420, ALP 187287, and Total bilirubin 0.8 1.1).
A PET scan during admission showed non-specific lymphadenopathy in the thorax, abdomen, and pelvis, with a qEBV level of 2,518 IU/mL. Biopsies of a cervical lymph node and liver were performed. The liver biopsy indicated severe bile duct injury, and endotheliitis suggesting SACR. The cervical lymph node biopsy showed follicular hyperplasia with numerous EBV+ cells, consistent with early/non-destructive PTLD. After discussion with multiple specialists the patient was treated with three days of high-dose steroids for SACR. Shortly after IV steroid treatment, he was discharged with a steroid taper and his home IS regimen. Outpatient lab tests showed improved liver biochemistries but an acutely elevated EBV level to 10,252 IU/mL, concerning for rapidly progressing PTLD. He was seen by hematology and received four cycles of Rituximab for PTLD. Post-treatment, his EBV quantification was undetectable, and PET/CT demonstrated complete metabolic response.
Discussion: Our case illustrates the clinical conundrum where increased and decreased IS are simultaneously indicated, requiring individualized therapy. The use of high-dose steroids followed by Rituximab effectively managed both conditions.
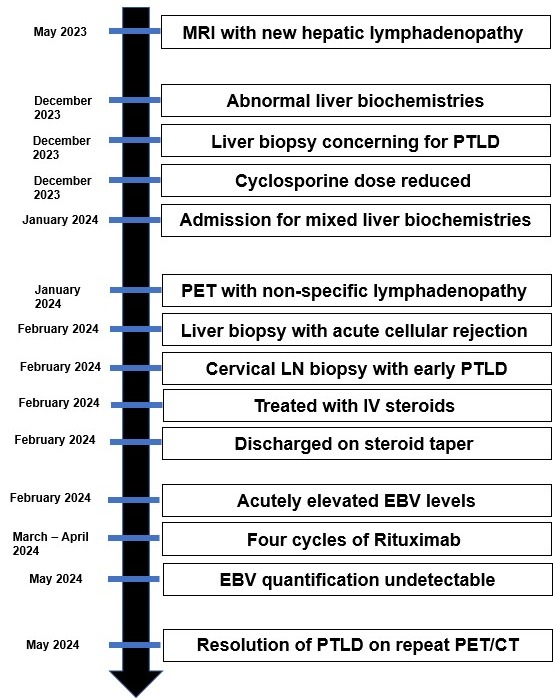
Figure: Figure 1. Timeline depicting clinical course and resolution of post-transplant lymphoproliferative disorder and acute cellular rejection.
Disclosures:
Ankit Mishra indicated no relevant financial relationships.
Priya Kathuria indicated no relevant financial relationships.
Dhiraj Peddu indicated no relevant financial relationships.
Matthew Kubina indicated no relevant financial relationships.
Hellan Kwon indicated no relevant financial relationships.
Shannon Carty indicated no relevant financial relationships.
Patricia Bloom indicated no relevant financial relationships.
Ankit Mishra, MD1, Priya Kathuria, MD1, Dhiraj Peddu, MD2, Matthew Kubina, MD1, Hellan Kwon, MD2, Shannon Carty, MD2, Patricia Bloom, MD2. P4731 - Simultaneous Presentation of Post-Transplant Lymphoproliferative Disorder (PTLD) and Acute Cellular Rejection (ACR) in a Liver Transplant Recipient: A Therapeutic Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
