Tuesday Poster Session
Category: Liver
P4734 - A Case of Variceal Bleeding Post-Whipple in a Patient Without Cirrhosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yende Grell, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Yende Grell, MD, Vladislav Fomin, MD, Catherine Lucero, MD
New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Portal vein thrombosis (PVT) and complications of portal hypertension (PH) such as variceal bleeding in the absence of cirrhosis can be seen in patients with hepatobiliary malignancy as sequelae of surgery. We present a case of variceal bleeding due to PVT after a pancreaticoduodenectomy (Whipple procedure) for cholangiocarcinoma.
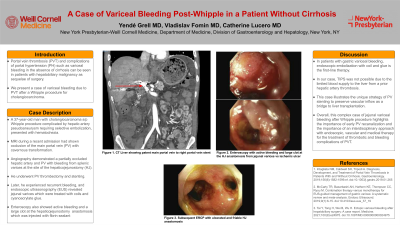
Case Description/Methods: A 37-year-old man with a history of primary sclerosing cholangitis and ulcerative colitis developed cholangiocarcinoma and was treated with gemcitabine/cisplatin/durvalumab, and local radiation therapy prior to his curative Whipple procedure that was complicated by hepatic artery pseudoaneurysm requiring selective embolization. He presented several months later with hematochezia. He initially presented at an outside institution for esophageal variceal bleeding treated with banding, and magnetic resonance imaging showed occlusion of the main portal vein (PV) with cavernous transformation. Angiography demonstrated a partially occluded hepatic artery and PV with bleeding from splenic varices at the site of the hepaticojejunostomy. He underwent PV thrombectomy and stenting. Later, he experienced recurrent bleeding, and endoscopic ultrasonography revealed jejunal varices, which were treated with coils and cyanoacrylate glue. He stabilized and remains on prophylactic anticoagulation (AC). He is currently listed for liver transplantation for recurrent variceal bleed without evidence of cancer recurrence.
Discussion: Early therapeutic AC should be initiated for acute PVT to prevent complete occlusion, cavernous transformation, and sequelae of PH. In patients with gastric variceal bleeding, endoscopic embolization with coil and glue is the first-line therapy. A patient with active bleeding not amenable to endoscopic intervention requires vascular recanalization such as transjugular intrahepatic portosystemic shunt (TIPS) and thrombectomy. In our case, TIPS was not possible due to the limited blood supply to the liver from a prior hepatic artery thrombosis. This case illustrates the unique strategy of PV stenting to preserve vascular inflow as a bridge to liver transplantation.
Overall, this complex case of jejunal variceal bleeding after Whipple procedure highlights the importance of early PV recanalization and the importance of an interdisciplinary approach with endoscopic, vascular and medical therapy for the treatment of thrombotic and bleeding complications of PVT.
Disclosures:
Yende Grell, MD, Vladislav Fomin, MD, Catherine Lucero, MD. P4734 - A Case of Variceal Bleeding Post-Whipple in a Patient Without Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Portal vein thrombosis (PVT) and complications of portal hypertension (PH) such as variceal bleeding in the absence of cirrhosis can be seen in patients with hepatobiliary malignancy as sequelae of surgery. We present a case of variceal bleeding due to PVT after a pancreaticoduodenectomy (Whipple procedure) for cholangiocarcinoma.
Case Description/Methods: A 37-year-old man with a history of primary sclerosing cholangitis and ulcerative colitis developed cholangiocarcinoma and was treated with gemcitabine/cisplatin/durvalumab, and local radiation therapy prior to his curative Whipple procedure that was complicated by hepatic artery pseudoaneurysm requiring selective embolization. He presented several months later with hematochezia. He initially presented at an outside institution for esophageal variceal bleeding treated with banding, and magnetic resonance imaging showed occlusion of the main portal vein (PV) with cavernous transformation. Angiography demonstrated a partially occluded hepatic artery and PV with bleeding from splenic varices at the site of the hepaticojejunostomy. He underwent PV thrombectomy and stenting. Later, he experienced recurrent bleeding, and endoscopic ultrasonography revealed jejunal varices, which were treated with coils and cyanoacrylate glue. He stabilized and remains on prophylactic anticoagulation (AC). He is currently listed for liver transplantation for recurrent variceal bleed without evidence of cancer recurrence.
Discussion: Early therapeutic AC should be initiated for acute PVT to prevent complete occlusion, cavernous transformation, and sequelae of PH. In patients with gastric variceal bleeding, endoscopic embolization with coil and glue is the first-line therapy. A patient with active bleeding not amenable to endoscopic intervention requires vascular recanalization such as transjugular intrahepatic portosystemic shunt (TIPS) and thrombectomy. In our case, TIPS was not possible due to the limited blood supply to the liver from a prior hepatic artery thrombosis. This case illustrates the unique strategy of PV stenting to preserve vascular inflow as a bridge to liver transplantation.
Overall, this complex case of jejunal variceal bleeding after Whipple procedure highlights the importance of early PV recanalization and the importance of an interdisciplinary approach with endoscopic, vascular and medical therapy for the treatment of thrombotic and bleeding complications of PVT.
Disclosures:
Yende Grell indicated no relevant financial relationships.
Vladislav Fomin indicated no relevant financial relationships.
Catherine Lucero indicated no relevant financial relationships.
Yende Grell, MD, Vladislav Fomin, MD, Catherine Lucero, MD. P4734 - A Case of Variceal Bleeding Post-Whipple in a Patient Without Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
