Tuesday Poster Session
Category: Liver
P4741 - A Rare Case of HSV Hepatitis and Peritonitis in a Post-Transplant Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AF
Aoife Feighery, MD
University of Cincinnati
Cincinnati, OH
Presenting Author(s)
Aoife Feighery, MD, Khurram Bari, MD
University of Cincinnati, Cincinnati, OH
Introduction: Herpes Simplex Virus (HSV) hepatitis is a rare entity, responsible for about 1% of all cases of acute liver failure (ALF), and 2% of viral-induced ALF. Sixty one percent of cases are from HSV2. Incidence is higher amongst the immunocompromised and pregnant women. Presentation is often non-specific. Fever is the most common symptom, seen in 98% of cases. Herpetic lesions are seen in only 44% of cases. Aminotransferases rise 100 to 1000 times the upper limit of normal, with a more pronounced AST elevation and relatively normal bilirubin (“anicteric hepatitis”). Leukopenia, thrombocytopenia, and renal failure are common. Gold standard for diagnosis is liver biopsy, however, over half of diagnoses are made post-mortem. Even amongst treated patients, rates of mortality or retransplant are over 50%.
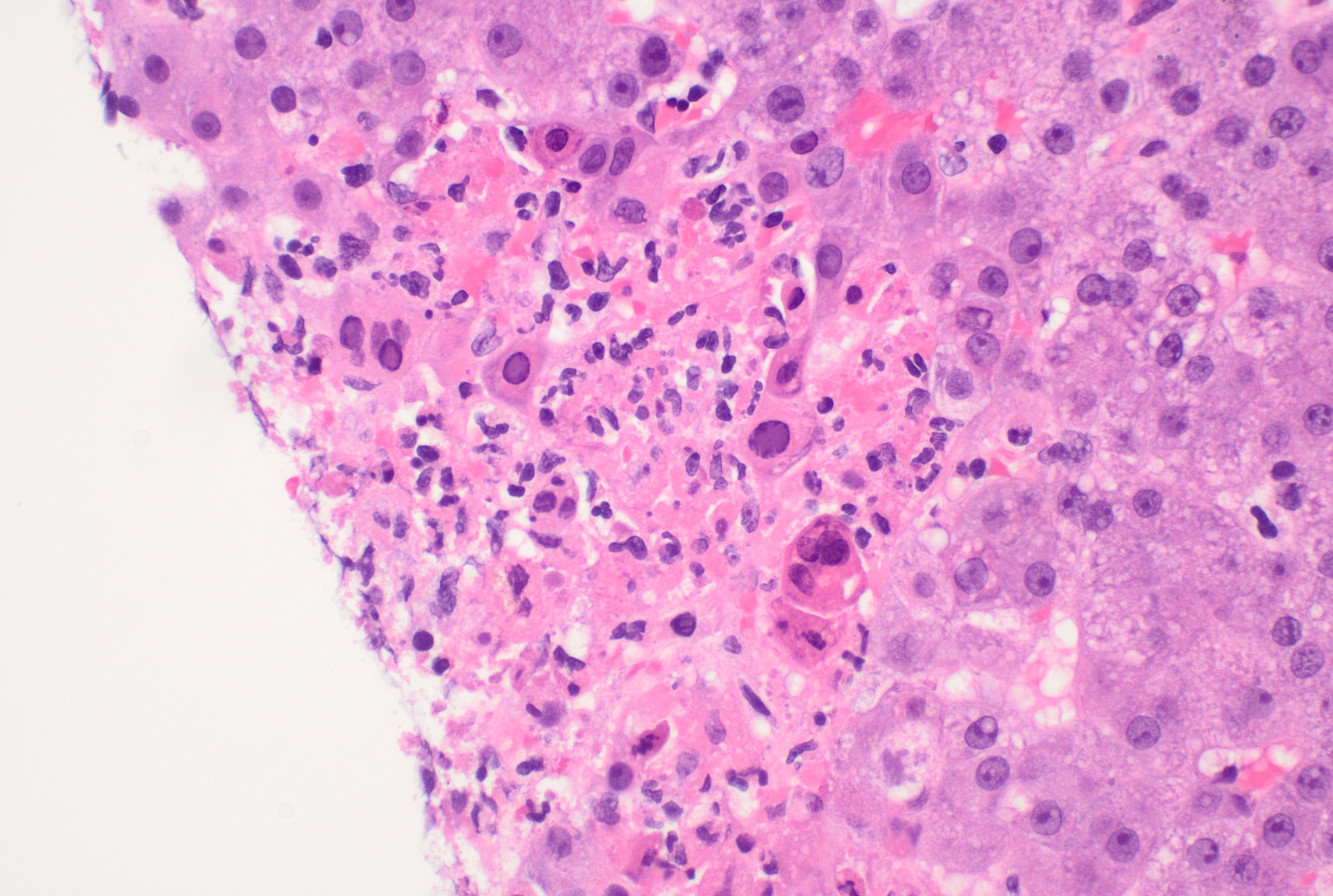
Case Description/Methods: A 55-year-old female, 18 months post-liver transplant, presented to the hospital with fevers of 39 C and severe abdominal pain. Prior transplant complications included delayed acute cellular rejection and post-transplant ascites. Her lab work was notable for AST 1100 U/L, ALT 500 U/L, ALP 200 U/L, total bilirubin 0.5 mg/dl. INR was normal and she had no evidence of encephalopathy. Complete blood count identified leukopenia (leucocytes 1.0 K/uL) and thrombocytopenia (platelets 72 K/uL). Renal panel revealed stage 2 AKI. She exhibited marked abdominal tenderness, but multiple scans ruled out surgical abdomen or vascular issues of the liver graft. She underwent diagnostic paracentesis with > 250 polymorphonuclear neutrophils. Due to concern for secondary bacterial peritonitis, she was started on piperacillin-tazobactam. She ultimately underwent liver biopsy which identified HSV-hepatitis with non-zonal confluent necrosis, up to 20% (Image 1). Serum HSV-2 PCR subsequently returned positive. Her ascitic fluid stained positive for HSV-2 as well. She was started on IV acyclovir and transitioned to oral valacyclovir before discharge.
Discussion: Here we present a rare case of post liver-transplant HSV hepatitis and peritonitis. HSV in post-liver transplant patients can mimic cholangitis, acute cellular rejection, or secondary peritonitis. Given the morbidity of HSV hepatitis, a high index of suspicion must be maintained for prompt diagnosis. In our patient, marked abdominal tenderness without a clear etiology on imaging, as well as the increased AST to ALT ratio were subtle clues. Fortunately, our patient responded well to therapy and her liver injury improved.
Disclosures:
Aoife Feighery, MD, Khurram Bari, MD. P4741 - A Rare Case of HSV Hepatitis and Peritonitis in a Post-Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Cincinnati, Cincinnati, OH
Introduction: Herpes Simplex Virus (HSV) hepatitis is a rare entity, responsible for about 1% of all cases of acute liver failure (ALF), and 2% of viral-induced ALF. Sixty one percent of cases are from HSV2. Incidence is higher amongst the immunocompromised and pregnant women. Presentation is often non-specific. Fever is the most common symptom, seen in 98% of cases. Herpetic lesions are seen in only 44% of cases. Aminotransferases rise 100 to 1000 times the upper limit of normal, with a more pronounced AST elevation and relatively normal bilirubin (“anicteric hepatitis”). Leukopenia, thrombocytopenia, and renal failure are common. Gold standard for diagnosis is liver biopsy, however, over half of diagnoses are made post-mortem. Even amongst treated patients, rates of mortality or retransplant are over 50%.
Case Description/Methods: A 55-year-old female, 18 months post-liver transplant, presented to the hospital with fevers of 39 C and severe abdominal pain. Prior transplant complications included delayed acute cellular rejection and post-transplant ascites. Her lab work was notable for AST 1100 U/L, ALT 500 U/L, ALP 200 U/L, total bilirubin 0.5 mg/dl. INR was normal and she had no evidence of encephalopathy. Complete blood count identified leukopenia (leucocytes 1.0 K/uL) and thrombocytopenia (platelets 72 K/uL). Renal panel revealed stage 2 AKI. She exhibited marked abdominal tenderness, but multiple scans ruled out surgical abdomen or vascular issues of the liver graft. She underwent diagnostic paracentesis with > 250 polymorphonuclear neutrophils. Due to concern for secondary bacterial peritonitis, she was started on piperacillin-tazobactam. She ultimately underwent liver biopsy which identified HSV-hepatitis with non-zonal confluent necrosis, up to 20% (Image 1). Serum HSV-2 PCR subsequently returned positive. Her ascitic fluid stained positive for HSV-2 as well. She was started on IV acyclovir and transitioned to oral valacyclovir before discharge.
Discussion: Here we present a rare case of post liver-transplant HSV hepatitis and peritonitis. HSV in post-liver transplant patients can mimic cholangitis, acute cellular rejection, or secondary peritonitis. Given the morbidity of HSV hepatitis, a high index of suspicion must be maintained for prompt diagnosis. In our patient, marked abdominal tenderness without a clear etiology on imaging, as well as the increased AST to ALT ratio were subtle clues. Fortunately, our patient responded well to therapy and her liver injury improved.
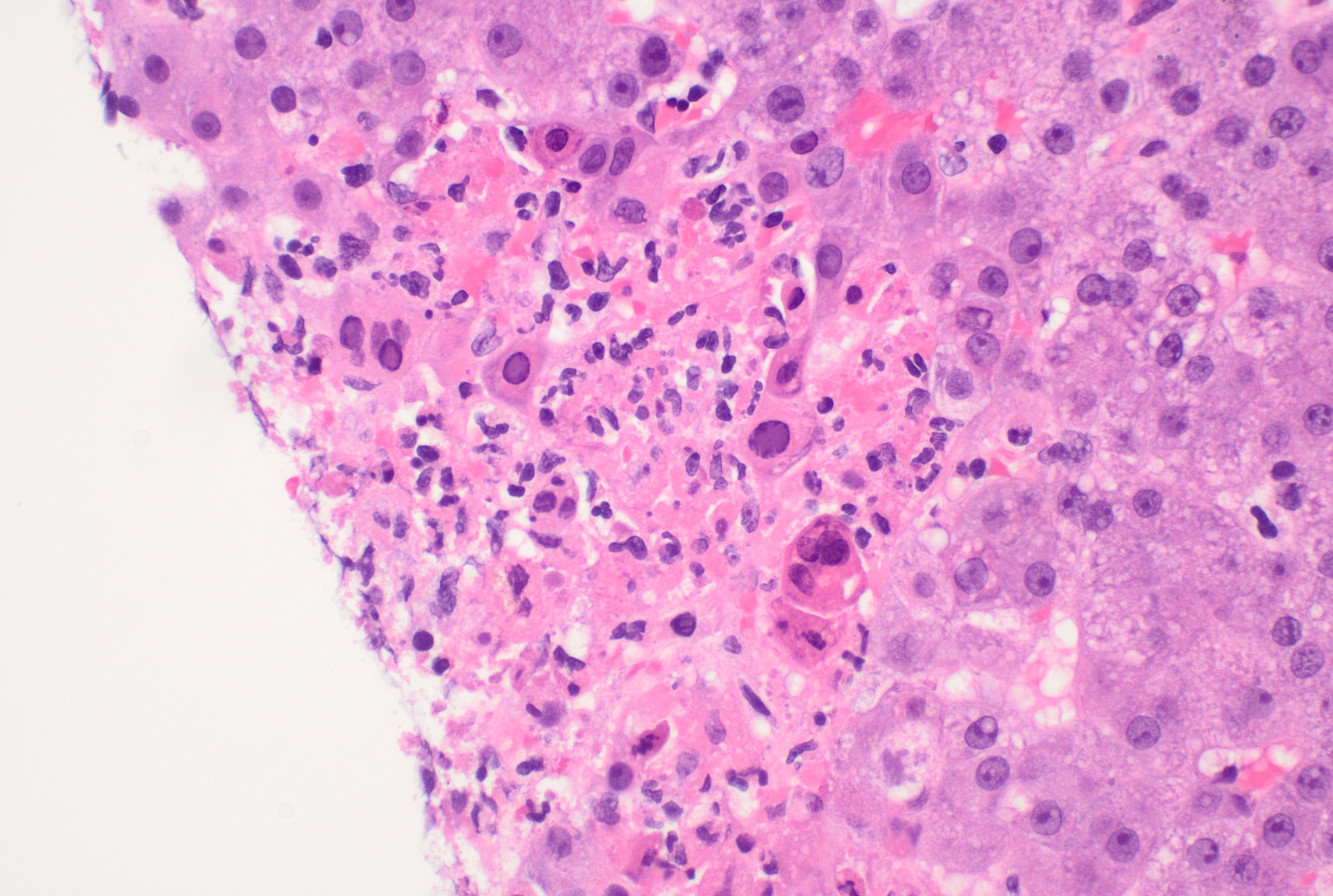
Figure: Image 1: Liver biopsy specimen showing viral cytopathic effect, as well as chromatin margination and multi-nucleation, characteristic of HSV hepatitis.
Disclosures:
Aoife Feighery indicated no relevant financial relationships.
Khurram Bari indicated no relevant financial relationships.
Aoife Feighery, MD, Khurram Bari, MD. P4741 - A Rare Case of HSV Hepatitis and Peritonitis in a Post-Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
