Tuesday Poster Session
Category: Liver
P4743 - Navigating Therapeutic Challenges in Metastatic Fibrolamellar Hepatocellular Carcinoma: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BD
Bassel Dakkak, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Bassel Dakkak, MD1, Omar Al Metwali, MBBCh1, Adamsegd I. Gebremedhen, MD1, Jennifer Wiese, MD2, Yasmeen Obeidat, MD1, Tejas Joshi, MD1
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Joan C. Edwards School of Medicine, Marshall University, Huntington, WV
Introduction: Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare liver cancer affecting young individuals without underlying liver disease. Treatment typically involves surgical resection, but some tumors are unresectable, and chemotherapy efficacy in such cases is limited. We present a case of a young male with metastatic, unresectable FLHCC, who was treated unsuccessfully with various chemotherapy regimens and a non-invasive technique called histiotripsy. This case highlights the importance of documenting all treatment attempts, especially novel methods like histiotripsy, to enhance understanding of emerging therapeutic options.
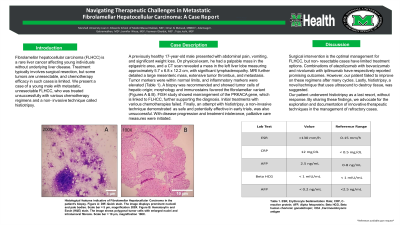
Case Description/Methods: A previously healthy 17-year-old male presented with abdominal pain, vomiting, and significant weight loss. He had no history of smoking, alcohol, or drug abuse, and no family history of liver diseases. On physical exam, he had a palpable mass in the epigastric area, and a CT scan revealed a mass in the left liver lobe measuring approximately 5.7 x 6.8 x 12.2 cm, with significant lymphadenopathy. MRI further detailed a large mesenteric mass, extensive tumor thrombus, and metastasis. Tumor markers were within normal limits, and inflammatory markers were elevated (Table 1). A biopsy was recommended and showed tumor cells of hepatic origin; morphology and immunostains favored the fibrolamellar variant (Figures 1 & 2). FISH study showed rearrangement of the PRKACA gene, which is linked to FLHCC, further supporting the diagnosis. Initial treatments with various chemotherapies failed. Finally, an attempt with histiotripsy, a non-invasive technique demonstrated as safe and potentially effective in early trials, was also unsuccessful. With disease progression and treatment intolerance, palliative care measures were initiated.
Discussion: Surgical intervention is the optimal management for FLHCC, but non-resectable cases have limited treatment options. Combinations of atezolizumab with bevacizumab and nivolumab with ipilimumab have respectively reported promising outcomes. However, our patient failed to improve on these regimens after many cycles. Lastly, histiotripsy, a novel technique that uses ultrasound to destroy tissue, was suggested. Our patient underwent histiotripsy as a last resort, without response. By sharing these findings we advocate for the exploration and documentation of innovative therapeutic techniques such as histiotripsy in the management of refractory cases.
ChatGPT improved grammar; content by authors.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bassel Dakkak, MD1, Omar Al Metwali, MBBCh1, Adamsegd I. Gebremedhen, MD1, Jennifer Wiese, MD2, Yasmeen Obeidat, MD1, Tejas Joshi, MD1. P4743 - Navigating Therapeutic Challenges in Metastatic Fibrolamellar Hepatocellular Carcinoma: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 2Joan C. Edwards School of Medicine, Marshall University, Huntington, WV
Introduction: Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare liver cancer affecting young individuals without underlying liver disease. Treatment typically involves surgical resection, but some tumors are unresectable, and chemotherapy efficacy in such cases is limited. We present a case of a young male with metastatic, unresectable FLHCC, who was treated unsuccessfully with various chemotherapy regimens and a non-invasive technique called histiotripsy. This case highlights the importance of documenting all treatment attempts, especially novel methods like histiotripsy, to enhance understanding of emerging therapeutic options.
Case Description/Methods: A previously healthy 17-year-old male presented with abdominal pain, vomiting, and significant weight loss. He had no history of smoking, alcohol, or drug abuse, and no family history of liver diseases. On physical exam, he had a palpable mass in the epigastric area, and a CT scan revealed a mass in the left liver lobe measuring approximately 5.7 x 6.8 x 12.2 cm, with significant lymphadenopathy. MRI further detailed a large mesenteric mass, extensive tumor thrombus, and metastasis. Tumor markers were within normal limits, and inflammatory markers were elevated (Table 1). A biopsy was recommended and showed tumor cells of hepatic origin; morphology and immunostains favored the fibrolamellar variant (Figures 1 & 2). FISH study showed rearrangement of the PRKACA gene, which is linked to FLHCC, further supporting the diagnosis. Initial treatments with various chemotherapies failed. Finally, an attempt with histiotripsy, a non-invasive technique demonstrated as safe and potentially effective in early trials, was also unsuccessful. With disease progression and treatment intolerance, palliative care measures were initiated.
Discussion: Surgical intervention is the optimal management for FLHCC, but non-resectable cases have limited treatment options. Combinations of atezolizumab with bevacizumab and nivolumab with ipilimumab have respectively reported promising outcomes. However, our patient failed to improve on these regimens after many cycles. Lastly, histiotripsy, a novel technique that uses ultrasound to destroy tissue, was suggested. Our patient underwent histiotripsy as a last resort, without response. By sharing these findings we advocate for the exploration and documentation of innovative therapeutic techniques such as histiotripsy in the management of refractory cases.
ChatGPT improved grammar; content by authors.

Figure: Histological features indicative of Fibrolamellar Hepatocellular Carcinoma in the patient's biopsy. Figure 1: Diff-Quick stain. The image displays prominent nucleoli and pale bodies. Scale bar = 5 μm, magnification 200X. Figure 2: Hematoxylin and Eosin (H&E) stain. The image shows polygonal tumor cells with enlarged nuclei and intratumoral fibrosis. Scale bar = 10 μm, magnification 100X.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bassel Dakkak indicated no relevant financial relationships.
Omar Al Metwali indicated no relevant financial relationships.
Adamsegd Gebremedhen indicated no relevant financial relationships.
Jennifer Wiese indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Tejas Joshi: Cook – Consultant. Echosens – Consultant. Gilead – Key Opinion Leader.
Bassel Dakkak, MD1, Omar Al Metwali, MBBCh1, Adamsegd I. Gebremedhen, MD1, Jennifer Wiese, MD2, Yasmeen Obeidat, MD1, Tejas Joshi, MD1. P4743 - Navigating Therapeutic Challenges in Metastatic Fibrolamellar Hepatocellular Carcinoma: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
