Tuesday Poster Session
Category: Liver
P4744 - Hemorrhagic Complication of an Ultrasound-Guided Paracentesis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- ES
Emily Seltzer, DO, MS
Memorial Sloan Kettering Cancer Center
New York, NY
Presenting Author(s)
Emily Seltzer, DO, MS1, Ines Varela Knorr, MD2, Walaa Mahmoud, MD3, Alexander Davidovich, DO, MSc4
1Memorial Sloan Kettering Cancer Center, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, New York, NY; 4Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Hemorrhage is a known, albeit infrequent, complication of paracenteses with a frequency of 2.2%. The use of ultrasound guidance decreases this risk to about 0.19%. We present a rare case of an injury to the deep circumflex iliac artery (DCIA) during an ultrasound-guided paracentesis.
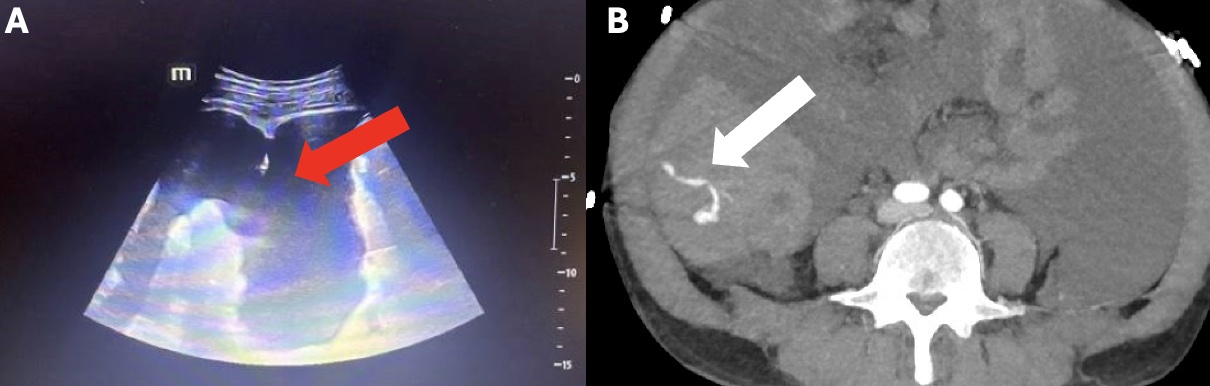
Case Description/Methods: A 61-year-old male with alcohol-associated cirrhosis complicated recurrent ascites requiring frequent paracenteses, presented with abdominal pain and shortness of breath. Vitals signs revealed normal blood pressure, heart rate tachycardic (105 bpm), and afebrile. His exam was pertinent for abdominal distension and lower extremity edema. His labs were notable for a hemoglobin of 9.4 g/dL (baseline), leukocytes of 6.9 × 109/L, INR of 1.4, with a MELD-Na of 10. An ultrasound-guided diagnostic and therapeutic paracentesis was performed using an 18-gauge introducer needle in the right lower quadrant (Image 1a). Two liters of cloudy-yellow fluid were removed. Several hours later, he developed abdominal pain without vital sign changes initially. The following morning, labs revealed a hemoglobin drop to 5.7 g/dL and new tachycardia to 110 bmp. A blood transfusion was ordered followed by a CT scan of the abdomen and pelvis. Upon returning from the scan, he was found pulseless in cardiac arrest. During the resuscitation, his hemoglobin was noted to be 3.8 g/dL and the CT scan revealed hyperattenuating material within the right hemiabdomen and pelvis compatible with hemoperitoneum. Massive transfusion protocol was initiated. Return of spontaneous circulation was obtained and the patient underwent an emergent CT angiography showing active extravasation (Image 1b). Interventional radiology performed an embolization targeted at the right DCIA. Despite all resuscitative efforts, the patient developed multiorgan failure and expired 24 hours later.
Discussion: Hemorrhage following injury to the DCIA after a paracentesis has been rarely reported. The damaged vessel often has a delayed presentation of hemorrhage without any visible hematoma. Thus, providers should maintain a high index of suspicion for post-procedure hemorrhagic complications. The use of Doppler imaging during paracenteses may be underutilized and integrating this into routine practice may decrease the risk of such complications.
Disclosures:
Emily Seltzer, DO, MS1, Ines Varela Knorr, MD2, Walaa Mahmoud, MD3, Alexander Davidovich, DO, MSc4. P4744 - Hemorrhagic Complication of an Ultrasound-Guided Paracentesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Memorial Sloan Kettering Cancer Center, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, New York, NY; 4Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Hemorrhage is a known, albeit infrequent, complication of paracenteses with a frequency of 2.2%. The use of ultrasound guidance decreases this risk to about 0.19%. We present a rare case of an injury to the deep circumflex iliac artery (DCIA) during an ultrasound-guided paracentesis.
Case Description/Methods: A 61-year-old male with alcohol-associated cirrhosis complicated recurrent ascites requiring frequent paracenteses, presented with abdominal pain and shortness of breath. Vitals signs revealed normal blood pressure, heart rate tachycardic (105 bpm), and afebrile. His exam was pertinent for abdominal distension and lower extremity edema. His labs were notable for a hemoglobin of 9.4 g/dL (baseline), leukocytes of 6.9 × 109/L, INR of 1.4, with a MELD-Na of 10. An ultrasound-guided diagnostic and therapeutic paracentesis was performed using an 18-gauge introducer needle in the right lower quadrant (Image 1a). Two liters of cloudy-yellow fluid were removed. Several hours later, he developed abdominal pain without vital sign changes initially. The following morning, labs revealed a hemoglobin drop to 5.7 g/dL and new tachycardia to 110 bmp. A blood transfusion was ordered followed by a CT scan of the abdomen and pelvis. Upon returning from the scan, he was found pulseless in cardiac arrest. During the resuscitation, his hemoglobin was noted to be 3.8 g/dL and the CT scan revealed hyperattenuating material within the right hemiabdomen and pelvis compatible with hemoperitoneum. Massive transfusion protocol was initiated. Return of spontaneous circulation was obtained and the patient underwent an emergent CT angiography showing active extravasation (Image 1b). Interventional radiology performed an embolization targeted at the right DCIA. Despite all resuscitative efforts, the patient developed multiorgan failure and expired 24 hours later.
Discussion: Hemorrhage following injury to the DCIA after a paracentesis has been rarely reported. The damaged vessel often has a delayed presentation of hemorrhage without any visible hematoma. Thus, providers should maintain a high index of suspicion for post-procedure hemorrhagic complications. The use of Doppler imaging during paracenteses may be underutilized and integrating this into routine practice may decrease the risk of such complications.
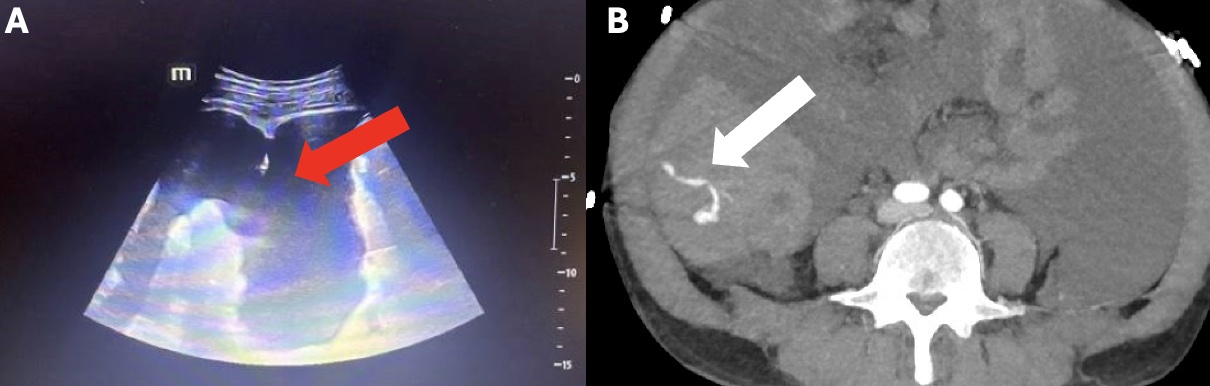
Figure: Image 1. A) Bedside ultrasound-guided paracentesis of the right lower quadrant with visible introducer tip within ascitic fluid (red arrow). 2) Computed tomography angiography scan of the abdomen and pelvis showing extravasation from the deep right circumflex artery (white arrow) with surrounding hemoperitoneum.
Disclosures:
Emily Seltzer indicated no relevant financial relationships.
Ines Varela Knorr indicated no relevant financial relationships.
Walaa Mahmoud indicated no relevant financial relationships.
Alexander Davidovich indicated no relevant financial relationships.
Emily Seltzer, DO, MS1, Ines Varela Knorr, MD2, Walaa Mahmoud, MD3, Alexander Davidovich, DO, MSc4. P4744 - Hemorrhagic Complication of an Ultrasound-Guided Paracentesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
