Tuesday Poster Session
Category: Liver
P4745 - Successful Use of Corticosteroids to Accelerate Recovery in Severe Autoimmune-like Hepatitis From Isoniazid: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Amir Sultan Seid, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Amir Sultan Seid, MD1, Oyedele Adeyi, MD1, Mary Thomson, MD, MSc2
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Corticosteroids have been used in some cases of drug-induced liver injury (DILI) to hasten recovery, although their efficacy remains controversial. We present a case of severe isoniazid (INH)-induced autoimmune-like hepatitis in which corticosteroid therapy was used to accelerate recovery following the discontinuation of INH.
Case Description/Methods: The patient is a 62-year-old U.S.-born man with a history of latent tuberculosis, primary progressive aphasia, and hypertension. He was initiated on INH because he had previously not tolerated rifampin. Two months after INH initiation, he presented to the hospital with jaundice, right upper quadrant abdominal pain, and fatigue. Initial laboratory tests revealed elevated liver enzymes (aspartate aminotransferase [AST] 2126 U/L, alanine aminotransferase [ALT] 2617 U/L) and bilirubin (total bilirubin 15.7 mg/dL, direct bilirubin 11.0 mg/dL). INR was 1.4. INH was promptly discontinued, and the patient was discharged with plan for outpatient follow up. However, he was readmitted a week later due to persistent jaundice. Repeat labs showed AST of 1623 U/L, ALT 2070 U/L, Bilirubin 17.5 mg/dl and INR of 1.37. Serologic tests for viral hepatitis (hepatitis A, hepatitis B, hepatitis C, cytomegalovirus, and Epstein-Barr), as well as autoimmune liver disease (antinuclear antibody, anti-smooth muscle antibody) were negative. Abdominal ultrasound with Doppler showed no evidence of biliary obstruction or hepatic vein thrombosis. A liver biopsy demonstrated severe acute hepatitis with features consistent with a drug-induced hypersensitivity reaction, including marked parenchymal lymphocytic and neutrophilic inflammation with multiple foci of interface and lobular confluent necrosis (Figure 1B). He was initiated on prednisone 40 mg daily to treat severe Isoniazid-induced autoimmune-like hepatitis. Within one week, he experienced a rapid improvement in bilirubin levels. Liver enzymes normalized over the following weeks, and prednisone was tapered off. At a 6-month follow-up visit, he remained asymptomatic with normal liver enzymes.
Discussion: Isoniazid hepatotoxicity is well known. INH should be used with caution in elderly patients, as they are at increased risk of liver injury. Corticosteroids should be considered in patients with drug-induce autoimmune-like hepatitis if they do not respond to drug withdrawal, but use in DILI from INH is controversial. This case illustrates the benefit of corticosteroids in severe autoimmune-like hepatitis from Isoniazid.

Disclosures:
Amir Sultan Seid, MD1, Oyedele Adeyi, MD1, Mary Thomson, MD, MSc2. P4745 - Successful Use of Corticosteroids to Accelerate Recovery in Severe Autoimmune-like Hepatitis From Isoniazid: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Corticosteroids have been used in some cases of drug-induced liver injury (DILI) to hasten recovery, although their efficacy remains controversial. We present a case of severe isoniazid (INH)-induced autoimmune-like hepatitis in which corticosteroid therapy was used to accelerate recovery following the discontinuation of INH.
Case Description/Methods: The patient is a 62-year-old U.S.-born man with a history of latent tuberculosis, primary progressive aphasia, and hypertension. He was initiated on INH because he had previously not tolerated rifampin. Two months after INH initiation, he presented to the hospital with jaundice, right upper quadrant abdominal pain, and fatigue. Initial laboratory tests revealed elevated liver enzymes (aspartate aminotransferase [AST] 2126 U/L, alanine aminotransferase [ALT] 2617 U/L) and bilirubin (total bilirubin 15.7 mg/dL, direct bilirubin 11.0 mg/dL). INR was 1.4. INH was promptly discontinued, and the patient was discharged with plan for outpatient follow up. However, he was readmitted a week later due to persistent jaundice. Repeat labs showed AST of 1623 U/L, ALT 2070 U/L, Bilirubin 17.5 mg/dl and INR of 1.37. Serologic tests for viral hepatitis (hepatitis A, hepatitis B, hepatitis C, cytomegalovirus, and Epstein-Barr), as well as autoimmune liver disease (antinuclear antibody, anti-smooth muscle antibody) were negative. Abdominal ultrasound with Doppler showed no evidence of biliary obstruction or hepatic vein thrombosis. A liver biopsy demonstrated severe acute hepatitis with features consistent with a drug-induced hypersensitivity reaction, including marked parenchymal lymphocytic and neutrophilic inflammation with multiple foci of interface and lobular confluent necrosis (Figure 1B). He was initiated on prednisone 40 mg daily to treat severe Isoniazid-induced autoimmune-like hepatitis. Within one week, he experienced a rapid improvement in bilirubin levels. Liver enzymes normalized over the following weeks, and prednisone was tapered off. At a 6-month follow-up visit, he remained asymptomatic with normal liver enzymes.
Discussion: Isoniazid hepatotoxicity is well known. INH should be used with caution in elderly patients, as they are at increased risk of liver injury. Corticosteroids should be considered in patients with drug-induce autoimmune-like hepatitis if they do not respond to drug withdrawal, but use in DILI from INH is controversial. This case illustrates the benefit of corticosteroids in severe autoimmune-like hepatitis from Isoniazid.

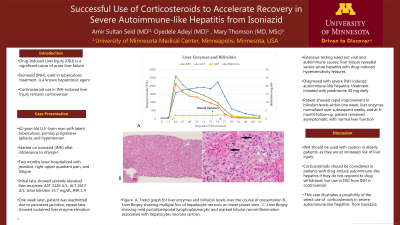
Figure: Figure 1
A. Trend graph for liver enzymes and bilirubin levels over the course of presentation
B. Liver Biopsy showing multiple foci of hepatocyte necrosis on lower power view. Hematoxylin & eosin stain, original magnification 100x
C. Liver Biopsy showing mild portal/periportal lymphoplasmacytic and marked lobular necroinflammation associated with hepatocytes necrosis (arrow). Hematoxylin & eosin stain, original magnification 200x.
A. Trend graph for liver enzymes and bilirubin levels over the course of presentation
B. Liver Biopsy showing multiple foci of hepatocyte necrosis on lower power view. Hematoxylin & eosin stain, original magnification 100x
C. Liver Biopsy showing mild portal/periportal lymphoplasmacytic and marked lobular necroinflammation associated with hepatocytes necrosis (arrow). Hematoxylin & eosin stain, original magnification 200x.
Disclosures:
Amir Sultan Seid indicated no relevant financial relationships.
Oyedele Adeyi indicated no relevant financial relationships.
Mary Thomson indicated no relevant financial relationships.
Amir Sultan Seid, MD1, Oyedele Adeyi, MD1, Mary Thomson, MD, MSc2. P4745 - Successful Use of Corticosteroids to Accelerate Recovery in Severe Autoimmune-like Hepatitis From Isoniazid: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
