Tuesday Poster Session
Category: Liver
P4747 - Invasive Liver Abscess Syndrome Predisposed by Klebsiella Pneumoniae-Related Prostate Abscess in a Nondiabetic Patient: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Sushil Rayamajhi, MD
University of Central Florida, HCA Healthcare GME
Pensacola, FL
Presenting Author(s)
Sushil Rayamajhi, MD1, Jun Yoo, DO1, Pradeep Kumari, MD2, Colton Boney, DO3, Anil Harrison, MD1
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Gulf Coast Infectious Disease, Pensacola, FL; 3University of South Alabama College of Medicine, Pensacola, FL
Introduction: Invasive liver abscess syndrome is characterized by the isolation of K. pneumoniae from the abscess aspirate or blood in patients who have imaging-confirmed liver abscesses, without any preexisting hepatobiliary disease. Prostate abscesses often arise as complications of acute urinary tract infections. Instances of concurrent pyogenic liver and prostate abscesses are very rare.
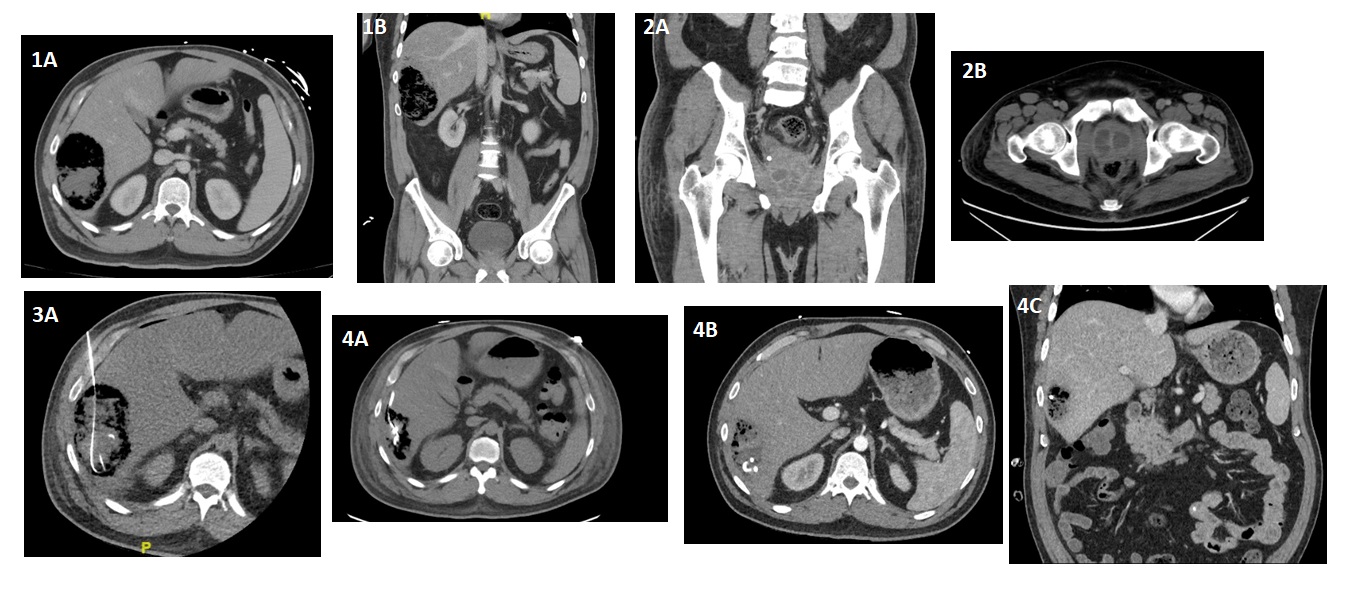
Case Description/Methods: We present a rare case of a 47-year-old non-diabetic male who presented to our hospital with complaints of generalized malaise, right abdomen fullness with pain, nausea, vomiting, urinary frequency and nocturia. CT abdomen/pelvis revealed a large non-ruptured liver abscess measuring 10.1 cm*6.2 cm*10.7 cm and prostate abscess with prostatomegaly. Liver abscess was drained with CT guided catheter placement into right hepatic lobe abscess. PCR of abscess aspirate blood culture and urine cultures confirmed K. pneumoniae, diagnosing him with invasive liver abscess syndrome. He was effectively treated with pigtail catheter drainage and six-week course of antibiotics.
Discussion: Invasive liver abscess syndrome is characterized by the isolation of K. pneumoniae from the abscess aspirate or blood in patients who have imaging-confirmed liver abscesses, without any preexisting hepatobiliary disease. Although diabetes is commonly associated with K. pneumoniae liver abscesses, our patient did not have this particular risk factor. Six independent risk factors have been proposed predicting severe complications of K. pneumoniae liver abscess including: thrombocytopenia (< 100,000/mm3), alkaline phosphatase >300 U/L, gas formation in the abscess, APACHE III score >40, use of cefazolin (instead of extended spectrum cephalosporin), and delayed drainage. The initial platelet count in our patient was 62,000/mm3 with alkaline phosphatase of 542 U/L, and delayed drainage contributed to progression of the invasive liver abscess syndrome. Apart from empirical antibiotic treatment, pigtail catheter drainage is the primary treatment strategy for liver abscesses. The patient was treated successfully with catheter drainage and six-week course of antibiotics. This case contributes to the limited literature on K. pneumonia invasive syndrome with liver abscess and prostatitis. This case highlights the critical need for prompt and precise diagnosis followed by suitable aggressive treatment in cases of disseminated K. pneumoniae infection to mitigate significant morbidity and mortality.
Disclosures:
Sushil Rayamajhi, MD1, Jun Yoo, DO1, Pradeep Kumari, MD2, Colton Boney, DO3, Anil Harrison, MD1. P4747 - Invasive Liver Abscess Syndrome Predisposed by Klebsiella Pneumoniae-Related Prostate Abscess in a Nondiabetic Patient: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Gulf Coast Infectious Disease, Pensacola, FL; 3University of South Alabama College of Medicine, Pensacola, FL
Introduction: Invasive liver abscess syndrome is characterized by the isolation of K. pneumoniae from the abscess aspirate or blood in patients who have imaging-confirmed liver abscesses, without any preexisting hepatobiliary disease. Prostate abscesses often arise as complications of acute urinary tract infections. Instances of concurrent pyogenic liver and prostate abscesses are very rare.
Case Description/Methods: We present a rare case of a 47-year-old non-diabetic male who presented to our hospital with complaints of generalized malaise, right abdomen fullness with pain, nausea, vomiting, urinary frequency and nocturia. CT abdomen/pelvis revealed a large non-ruptured liver abscess measuring 10.1 cm*6.2 cm*10.7 cm and prostate abscess with prostatomegaly. Liver abscess was drained with CT guided catheter placement into right hepatic lobe abscess. PCR of abscess aspirate blood culture and urine cultures confirmed K. pneumoniae, diagnosing him with invasive liver abscess syndrome. He was effectively treated with pigtail catheter drainage and six-week course of antibiotics.
Discussion: Invasive liver abscess syndrome is characterized by the isolation of K. pneumoniae from the abscess aspirate or blood in patients who have imaging-confirmed liver abscesses, without any preexisting hepatobiliary disease. Although diabetes is commonly associated with K. pneumoniae liver abscesses, our patient did not have this particular risk factor. Six independent risk factors have been proposed predicting severe complications of K. pneumoniae liver abscess including: thrombocytopenia (< 100,000/mm3), alkaline phosphatase >300 U/L, gas formation in the abscess, APACHE III score >40, use of cefazolin (instead of extended spectrum cephalosporin), and delayed drainage. The initial platelet count in our patient was 62,000/mm3 with alkaline phosphatase of 542 U/L, and delayed drainage contributed to progression of the invasive liver abscess syndrome. Apart from empirical antibiotic treatment, pigtail catheter drainage is the primary treatment strategy for liver abscesses. The patient was treated successfully with catheter drainage and six-week course of antibiotics. This case contributes to the limited literature on K. pneumonia invasive syndrome with liver abscess and prostatitis. This case highlights the critical need for prompt and precise diagnosis followed by suitable aggressive treatment in cases of disseminated K. pneumoniae infection to mitigate significant morbidity and mortality.
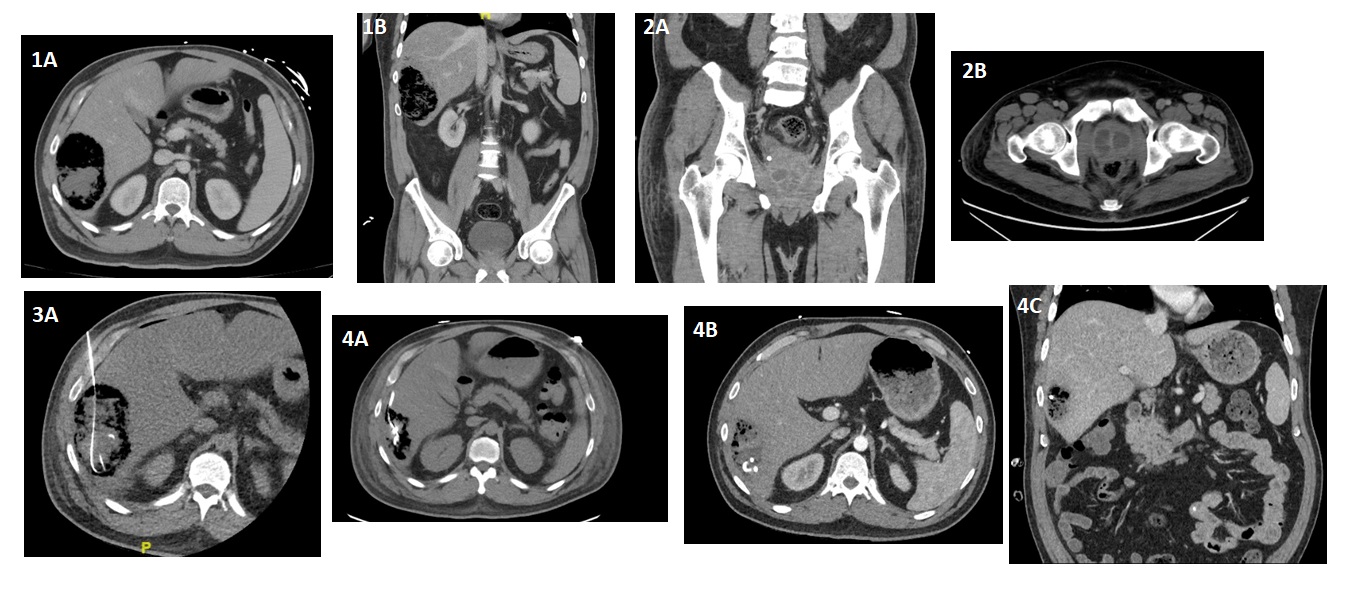
Figure: 1A, 1B. CT abdomen/pelvis revealed a large non-ruptured liver abscess measuring 10.1 cm*6.2 cm*10.7 cm
2A, 2B. CT abdomen/pelvis revealed prostatomegaly with the appearance of low attenuated densities bilaterally, approximately 3.4 x 1.9 on the right and 2.0 x 2.0 on the left with presacral soft tissue infiltration representing prostate abscess
3A. Successful CT guided 10 French drainage catheter placement into right hepatic lobe abscess
4A, 4B, 4C. Resolving complex right hepatic abscess, well positioned percutaneous catheter
2A, 2B. CT abdomen/pelvis revealed prostatomegaly with the appearance of low attenuated densities bilaterally, approximately 3.4 x 1.9 on the right and 2.0 x 2.0 on the left with presacral soft tissue infiltration representing prostate abscess
3A. Successful CT guided 10 French drainage catheter placement into right hepatic lobe abscess
4A, 4B, 4C. Resolving complex right hepatic abscess, well positioned percutaneous catheter
Disclosures:
Sushil Rayamajhi indicated no relevant financial relationships.
Jun Yoo indicated no relevant financial relationships.
Pradeep Kumari indicated no relevant financial relationships.
Colton Boney indicated no relevant financial relationships.
Anil Harrison indicated no relevant financial relationships.
Sushil Rayamajhi, MD1, Jun Yoo, DO1, Pradeep Kumari, MD2, Colton Boney, DO3, Anil Harrison, MD1. P4747 - Invasive Liver Abscess Syndrome Predisposed by Klebsiella Pneumoniae-Related Prostate Abscess in a Nondiabetic Patient: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
