Tuesday Poster Session
Category: Liver
P4781 - A Rare Case of Piggyback Syndrome Following Orthotopic Liver Transplant
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kelvin Liao, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Kelvin Liao, MD, Neha Jakhete, MD
University of Maryland Medical Center, Baltimore, MD
Introduction: Piggyback syndrome is a rare complication of orthotopic liver transplant (OLT) performed via the piggyback technique. Where conventional OLT involves anastomosis of both the donor and recipient inferior vena cava (IVC), piggyback OLT instead creates anastomoses between the donor IVC and recipient hepatic veins. Piggyback syndrome describes the sequelae of hepatic vein outflow obstruction arising from anastomotic stenosis following piggyback OLT. We present a case of piggyback syndrome successfully treated with percutaneous stenting and balloon angioplasty.
Case Description/Methods: A 46-year-old male with alcohol use disorder presented with progressive abdominal distention and lower extremity edema. Five months ago, he underwent OLT performed via piggyback technique for acute on chronic liver failure due to alcoholic cirrhosis.
Magnetic Resonance Imaging (MRI) of the abdomen revealed new hepatomegaly and large volume ascites without liver lesions or biliary ductal dilation. Paracentesis yielded fluid with total protein 2.9g/dL and a high serum albumin-ascites gradient of 1.5g/dL. Echocardiogram showed normal biventricular function. Doppler ultrasound of the hepatic vasculature in decubitus, supine, and upright positions showed persistently decreased cardiac phasicity in the middle hepatic vein anastomosis. Transjugular liver biopsy revealed sinusoidal dilatation and a hepatic venous pressure gradient of 26mmhg consistent with venous outflow obstruction. There was no evidence of acute cellular rejection.
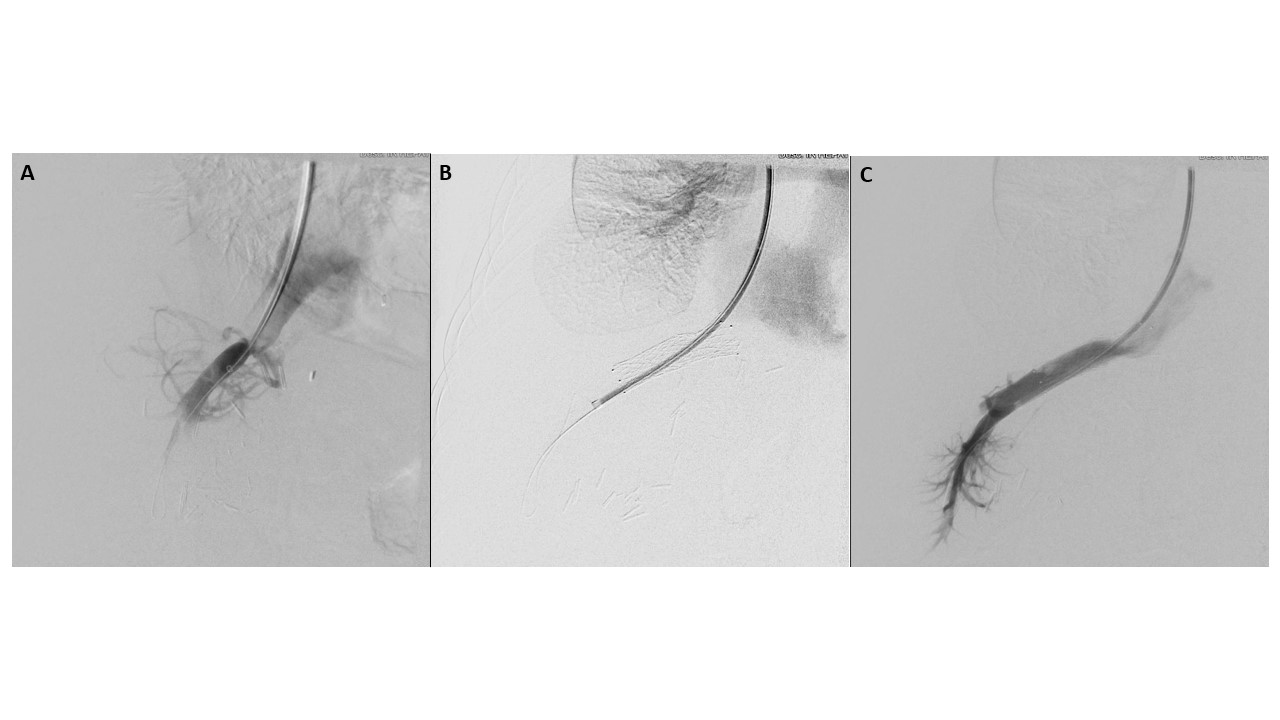
Hepatic venogram revealed moderate to severe stenosis of the middle hepatic vein. An uncovered stent was deployed across the stenotic area extending from the middle hepatic vein anastomosis to the IVC. Balloon venoplasty of the stent was then performed. Post-procedural venogram demonstrated patency of the piggyback anastomosis.
The patient remained without ascites and with normal liver-associated enzymes at one, two, three, six, and twelve month follow ups.
Discussion: Piggyback syndrome is a rare complication of piggyback OLT and involves anastomotic stricture resulting in obstructed hepatic vein outflow. Incidence is estimated at 0.8%-1%. Piggyback syndrome may be mistaken for acute rejection therefore detailed evaluation with cross-sectional imaging, liver biopsy, and hepatic venogram should be undertaken to differentiate the two processes. Percutaneous stenting and balloon angioplasty are minimally invasive, safe, and effective techniques to alleviate anastomotic strictures.
Disclosures:
Kelvin Liao, MD, Neha Jakhete, MD. P4781 - A Rare Case of Piggyback Syndrome Following Orthotopic Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Maryland Medical Center, Baltimore, MD
Introduction: Piggyback syndrome is a rare complication of orthotopic liver transplant (OLT) performed via the piggyback technique. Where conventional OLT involves anastomosis of both the donor and recipient inferior vena cava (IVC), piggyback OLT instead creates anastomoses between the donor IVC and recipient hepatic veins. Piggyback syndrome describes the sequelae of hepatic vein outflow obstruction arising from anastomotic stenosis following piggyback OLT. We present a case of piggyback syndrome successfully treated with percutaneous stenting and balloon angioplasty.
Case Description/Methods: A 46-year-old male with alcohol use disorder presented with progressive abdominal distention and lower extremity edema. Five months ago, he underwent OLT performed via piggyback technique for acute on chronic liver failure due to alcoholic cirrhosis.
Magnetic Resonance Imaging (MRI) of the abdomen revealed new hepatomegaly and large volume ascites without liver lesions or biliary ductal dilation. Paracentesis yielded fluid with total protein 2.9g/dL and a high serum albumin-ascites gradient of 1.5g/dL. Echocardiogram showed normal biventricular function. Doppler ultrasound of the hepatic vasculature in decubitus, supine, and upright positions showed persistently decreased cardiac phasicity in the middle hepatic vein anastomosis. Transjugular liver biopsy revealed sinusoidal dilatation and a hepatic venous pressure gradient of 26mmhg consistent with venous outflow obstruction. There was no evidence of acute cellular rejection.
Hepatic venogram revealed moderate to severe stenosis of the middle hepatic vein. An uncovered stent was deployed across the stenotic area extending from the middle hepatic vein anastomosis to the IVC. Balloon venoplasty of the stent was then performed. Post-procedural venogram demonstrated patency of the piggyback anastomosis.
The patient remained without ascites and with normal liver-associated enzymes at one, two, three, six, and twelve month follow ups.
Discussion: Piggyback syndrome is a rare complication of piggyback OLT and involves anastomotic stricture resulting in obstructed hepatic vein outflow. Incidence is estimated at 0.8%-1%. Piggyback syndrome may be mistaken for acute rejection therefore detailed evaluation with cross-sectional imaging, liver biopsy, and hepatic venogram should be undertaken to differentiate the two processes. Percutaneous stenting and balloon angioplasty are minimally invasive, safe, and effective techniques to alleviate anastomotic strictures.
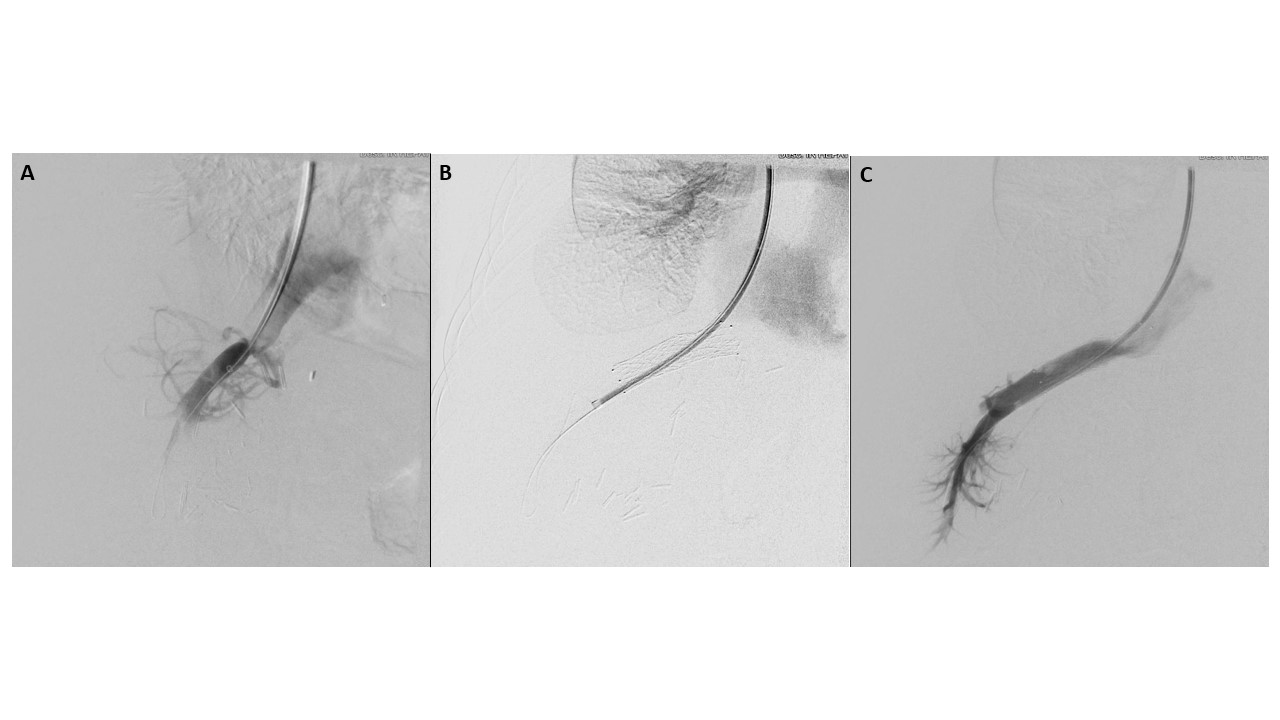
Figure: Figure 1. (A) Cannulation of the middle hepatic vein-IVC anastomosis with lack of distal opacification consistent with severe stenosis. (B) Placement of uncovered metal stent across the middle hepatic vein-IVC anastomosis. (C) Post-stenting venogram with robust opacification distal to the anastomosis.
Disclosures:
Kelvin Liao indicated no relevant financial relationships.
Neha Jakhete indicated no relevant financial relationships.
Kelvin Liao, MD, Neha Jakhete, MD. P4781 - A Rare Case of Piggyback Syndrome Following Orthotopic Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
