Tuesday Poster Session
Category: Liver
P4788 - Extramedullary Hematopoiesis: An Unusual Cause of Ascites in a Post-Liver Transplant Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Leo Kleyman, MD
Baylor College of Medicine
Miami, FL
Presenting Author(s)
Leo Kleyman, MD1, Sally Condon, MD2, David S. Lessen, MD, MBA3, Yamilé Blain, MD4, Nemencio Ronquillo, MD2, Patricia Jones, MD, MSCR2
1Baylor College of Medicine, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL; 3University of Miami Miller School of Medicine, Deerfield Beach, FL; 4University of Miami Health System, Miami, FL
Introduction: Portal hypertension can be categorized into pre-hepatic, intrahepatic and post hepatic causes. We present a case of a patient who underwent liver transplant secondary to Budd-Chiari syndrome and presented with ascites, thrombocytopenia and splenomegaly 31 years post-transplant. While cirrhosis of the transplanted liver was the leading diagnostic consideration, biopsy revealed extramedullary hematopoiesis (EMH), a known complication of myelofibrosis (MF), with resultant noncirrhotic portal hypertension.
Case Description/Methods: A 63 y/o patient with JAK-2 positive polycythemia vera (PV) developed Budd-Chiari Syndrome necessitating liver transplant in 1992. She required kidney transplant in 2009 for calcineurin inhibitor toxicity. Current immunosuppression includes mycophenolate mofetil and tacrolimus. For PV, she was maintained on hydroxyurea and regular phlebotomy. In late 2023, she had progressive thrombocytopenia, and imaging showed massive splenomegaly with splenic varices. Bone marrow biopsy (BMBx) was consistent with PV with notation of MF-1 fibrosis. Thrombocytopenia was thought to be multifactorial, due to splenic sequestration and as an adverse effect of hydroxyurea. In this context and with mildly elevated transaminases, a hepatology consult was initiated.
Prior to Hepatology visit, she presented to the emergency room with acute RUQ abdominal pain and was noted to have ascites. An extensive infectious work-up was negative and liver biopsy was recommended to rule out recurrent graft cirrhosis vs. noncirrhotic portal hypertension. Transjugular liver biopsy demonstrated marked sinusoidal EMH, and focal centrilobular perisinusoidal fibrosis without evidence of chronic ductopenic rejection; EMH is exceedingly rare in PV and is more commonly associated with MF. Subsequently, repeat BMBx demonstrated progression to post-PV MF (WHO MF-2). Abdominal pain was ultimately controlled with oral analgesics. Thrombocytopenia improved slightly with reduced hydroxyurea dose.
Discussion: This case highlights EMH, a rare cause of portal hypertension. This transplant patient presented with seemingly classical signs of decompensated cirrhosis, yet her biopsy demonstrated profound EMH with no evidence of chronic rejection. Even in the setting of concerns for rejection or liver dysfunction, causes of noncirrhotic portal hypertension should be investigated, especially in patients with underlying hematologic diseases or malignancies, such as PV or MF.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Leo Kleyman, MD1, Sally Condon, MD2, David S. Lessen, MD, MBA3, Yamilé Blain, MD4, Nemencio Ronquillo, MD2, Patricia Jones, MD, MSCR2. P4788 - Extramedullary Hematopoiesis: An Unusual Cause of Ascites in a Post-Liver Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor College of Medicine, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL; 3University of Miami Miller School of Medicine, Deerfield Beach, FL; 4University of Miami Health System, Miami, FL
Introduction: Portal hypertension can be categorized into pre-hepatic, intrahepatic and post hepatic causes. We present a case of a patient who underwent liver transplant secondary to Budd-Chiari syndrome and presented with ascites, thrombocytopenia and splenomegaly 31 years post-transplant. While cirrhosis of the transplanted liver was the leading diagnostic consideration, biopsy revealed extramedullary hematopoiesis (EMH), a known complication of myelofibrosis (MF), with resultant noncirrhotic portal hypertension.
Case Description/Methods: A 63 y/o patient with JAK-2 positive polycythemia vera (PV) developed Budd-Chiari Syndrome necessitating liver transplant in 1992. She required kidney transplant in 2009 for calcineurin inhibitor toxicity. Current immunosuppression includes mycophenolate mofetil and tacrolimus. For PV, she was maintained on hydroxyurea and regular phlebotomy. In late 2023, she had progressive thrombocytopenia, and imaging showed massive splenomegaly with splenic varices. Bone marrow biopsy (BMBx) was consistent with PV with notation of MF-1 fibrosis. Thrombocytopenia was thought to be multifactorial, due to splenic sequestration and as an adverse effect of hydroxyurea. In this context and with mildly elevated transaminases, a hepatology consult was initiated.
Prior to Hepatology visit, she presented to the emergency room with acute RUQ abdominal pain and was noted to have ascites. An extensive infectious work-up was negative and liver biopsy was recommended to rule out recurrent graft cirrhosis vs. noncirrhotic portal hypertension. Transjugular liver biopsy demonstrated marked sinusoidal EMH, and focal centrilobular perisinusoidal fibrosis without evidence of chronic ductopenic rejection; EMH is exceedingly rare in PV and is more commonly associated with MF. Subsequently, repeat BMBx demonstrated progression to post-PV MF (WHO MF-2). Abdominal pain was ultimately controlled with oral analgesics. Thrombocytopenia improved slightly with reduced hydroxyurea dose.
Discussion: This case highlights EMH, a rare cause of portal hypertension. This transplant patient presented with seemingly classical signs of decompensated cirrhosis, yet her biopsy demonstrated profound EMH with no evidence of chronic rejection. Even in the setting of concerns for rejection or liver dysfunction, causes of noncirrhotic portal hypertension should be investigated, especially in patients with underlying hematologic diseases or malignancies, such as PV or MF.

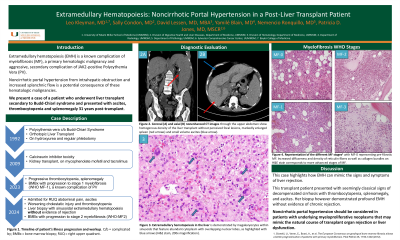
Figure: Figure 1. Coronal (A) and axial (B) nonenhanced CT images through the upper abdomen show homogenous density of the liver transplant without perceived focal lesions, markedly enlarged spleen and small volume ascites.
Figure 2. Extramedullary hematopoiesis in the liver is demonstrated by megakaryocytes within sinusoids that feature abundant cytoplasm with overlapping nuclear lobes, as highlighted with yellow arrows (H&E stain, 200x magnification).
Figure 2. Extramedullary hematopoiesis in the liver is demonstrated by megakaryocytes within sinusoids that feature abundant cytoplasm with overlapping nuclear lobes, as highlighted with yellow arrows (H&E stain, 200x magnification).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Leo Kleyman indicated no relevant financial relationships.
Sally Condon indicated no relevant financial relationships.
David Lessen indicated no relevant financial relationships.
Yamilé Blain indicated no relevant financial relationships.
Nemencio Ronquillo indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Leo Kleyman, MD1, Sally Condon, MD2, David S. Lessen, MD, MBA3, Yamilé Blain, MD4, Nemencio Ronquillo, MD2, Patricia Jones, MD, MSCR2. P4788 - Extramedullary Hematopoiesis: An Unusual Cause of Ascites in a Post-Liver Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
