Tuesday Poster Session
Category: Liver
P4801 - Booch or Hooch: Excessive Kombucha Intake Mimicking Alcoholic Hepatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arvin Jeremy Tan, MD
University of Hawaii, John A. Burns School of Medicine
Honolulu, HI
Presenting Author(s)
Award: Presidential Poster Award
Arvin Jeremy Tan, MD1, Shanelle Katrina Tan, BS2, Kevin Nebrejas, MD1, Traci T. Murakami, MD, FACG3, Nour Hamade, MD4
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Santo Tomas, Manila, National Capital Region, Philippines; 3The Queen's Medical Center, Honolulu, HI; 4The Queen's Medical Center, Ewa Beach, HI
Introduction: Drug-induced liver injury (DILI) has an annual incidence of 15 to 20 per 100,000. Medications and herbal supplements are typical culprits. The presentation may range from asymptomatic to acute liver failure. Here, we report a case of a patient with DILI due to excessive consumption of Kombucha.
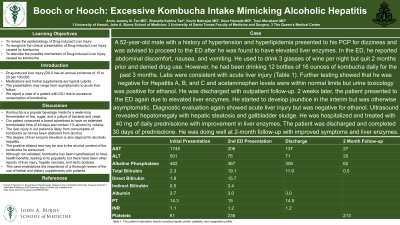
Case Description/Methods: A 52-year-old male with a history of hypertension and hyperlipidemia presented to the ED with elevated liver enzymes. He initially saw his PCP for dizziness and was advised to proceed to the ED after he was found to have elevated liver enzymes. In the ED, he reported that he has also been experiencing abdominal discomfort, nausea, and vomiting. He used to drink 3 glasses of wine per night but quit 2 months prior and denied drug use. However, he has been drinking 12 bottles of 16 ounces of kombucha daily for the past 3 months. Labs were consistent with acute liver injury (Table 1). Further testing showed that he was negative for Hepatitis A, B, and C and acetaminophen levels were within normal limits but urine toxicology was positive for ethanol. He was discharged with outpatient follow-up. 2 weeks later, the patient presented to the ED again due to elevated liver enzymes. He started to develop jaundice in the interim but was otherwise asymptomatic. Diagnostic evaluation again showed acute liver injury but was negative for ethanol. Ultrasound revealed hepatomegaly with hepatic steatosis and gallbladder sludge. He was hospitalized and treated with 40 mg of daily prednisolone with improvement in liver enzymes. The patient was discharged and completed 30 days of prednisolone. He was doing well at 2-month follow-up with improved symptoms and liver enzymes.
Discussion: Kombucha is a popular beverage made by a week-long fermentation of tea, sugar, and a culture of bacteria and yeast. Our patient consumed a brand advertised to have an extended fermentation time of 45 days and contain 1% alcohol by volume. The liver injury in our patient is likely from consumption of Kombucha as he has been abstinent from alcohol and the degree of liver enzyme elevation is atypical for alcoholic hepatitis. The positive ethanol test may be due to the alcohol content of the kombucha he consumed. Although not validated, Kombucha has been hypothesized to have health benefits, leading to its popularity, but there have been other reports of liver injury, hepatic necrosis, and lactic acidosis. It is hence important for providers to thoroughly review the use of herbal and dietary supplements with patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Arvin Jeremy Tan, MD1, Shanelle Katrina Tan, BS2, Kevin Nebrejas, MD1, Traci T. Murakami, MD, FACG3, Nour Hamade, MD4. P4801 - Booch or Hooch: Excessive Kombucha Intake Mimicking Alcoholic Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Arvin Jeremy Tan, MD1, Shanelle Katrina Tan, BS2, Kevin Nebrejas, MD1, Traci T. Murakami, MD, FACG3, Nour Hamade, MD4
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Santo Tomas, Manila, National Capital Region, Philippines; 3The Queen's Medical Center, Honolulu, HI; 4The Queen's Medical Center, Ewa Beach, HI
Introduction: Drug-induced liver injury (DILI) has an annual incidence of 15 to 20 per 100,000. Medications and herbal supplements are typical culprits. The presentation may range from asymptomatic to acute liver failure. Here, we report a case of a patient with DILI due to excessive consumption of Kombucha.
Case Description/Methods: A 52-year-old male with a history of hypertension and hyperlipidemia presented to the ED with elevated liver enzymes. He initially saw his PCP for dizziness and was advised to proceed to the ED after he was found to have elevated liver enzymes. In the ED, he reported that he has also been experiencing abdominal discomfort, nausea, and vomiting. He used to drink 3 glasses of wine per night but quit 2 months prior and denied drug use. However, he has been drinking 12 bottles of 16 ounces of kombucha daily for the past 3 months. Labs were consistent with acute liver injury (Table 1). Further testing showed that he was negative for Hepatitis A, B, and C and acetaminophen levels were within normal limits but urine toxicology was positive for ethanol. He was discharged with outpatient follow-up. 2 weeks later, the patient presented to the ED again due to elevated liver enzymes. He started to develop jaundice in the interim but was otherwise asymptomatic. Diagnostic evaluation again showed acute liver injury but was negative for ethanol. Ultrasound revealed hepatomegaly with hepatic steatosis and gallbladder sludge. He was hospitalized and treated with 40 mg of daily prednisolone with improvement in liver enzymes. The patient was discharged and completed 30 days of prednisolone. He was doing well at 2-month follow-up with improved symptoms and liver enzymes.
Discussion: Kombucha is a popular beverage made by a week-long fermentation of tea, sugar, and a culture of bacteria and yeast. Our patient consumed a brand advertised to have an extended fermentation time of 45 days and contain 1% alcohol by volume. The liver injury in our patient is likely from consumption of Kombucha as he has been abstinent from alcohol and the degree of liver enzyme elevation is atypical for alcoholic hepatitis. The positive ethanol test may be due to the alcohol content of the kombucha he consumed. Although not validated, Kombucha has been hypothesized to have health benefits, leading to its popularity, but there have been other reports of liver injury, hepatic necrosis, and lactic acidosis. It is hence important for providers to thoroughly review the use of herbal and dietary supplements with patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Arvin Jeremy Tan indicated no relevant financial relationships.
Shanelle Katrina Tan indicated no relevant financial relationships.
Kevin Nebrejas indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Nour Hamade indicated no relevant financial relationships.
Arvin Jeremy Tan, MD1, Shanelle Katrina Tan, BS2, Kevin Nebrejas, MD1, Traci T. Murakami, MD, FACG3, Nour Hamade, MD4. P4801 - Booch or Hooch: Excessive Kombucha Intake Mimicking Alcoholic Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

