Tuesday Poster Session
Category: Liver
P4802 - A Case of Primary Hepatic Small Cell Carcinoma Without Any Pulmonary Involvement: A Diagnostic Conundrum
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aboud Kaliounji, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Aboud Kaliounji, MD, Carla Hachicho, BA, Helena Saba, MD, Jude Noel, MD, Jenna Zudell, MD, Raavi Gupta, MD, Sushil Ahlawat, MD, MS, MBBS
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Extrapulmonary small cell carcinoma (EPSCC) are extremely rare and account for 2-4% of all small cell carcinoma (SCC) cases, and even rarer in the liver and biliary tract which have been previously described only in a few case reports over the past few decades. The clinical, pathological and immunohisotchemical properties of liver SCC are not fully established. We present a case of a female with primary liver SCC presenting with abdominal pain and vomiting.
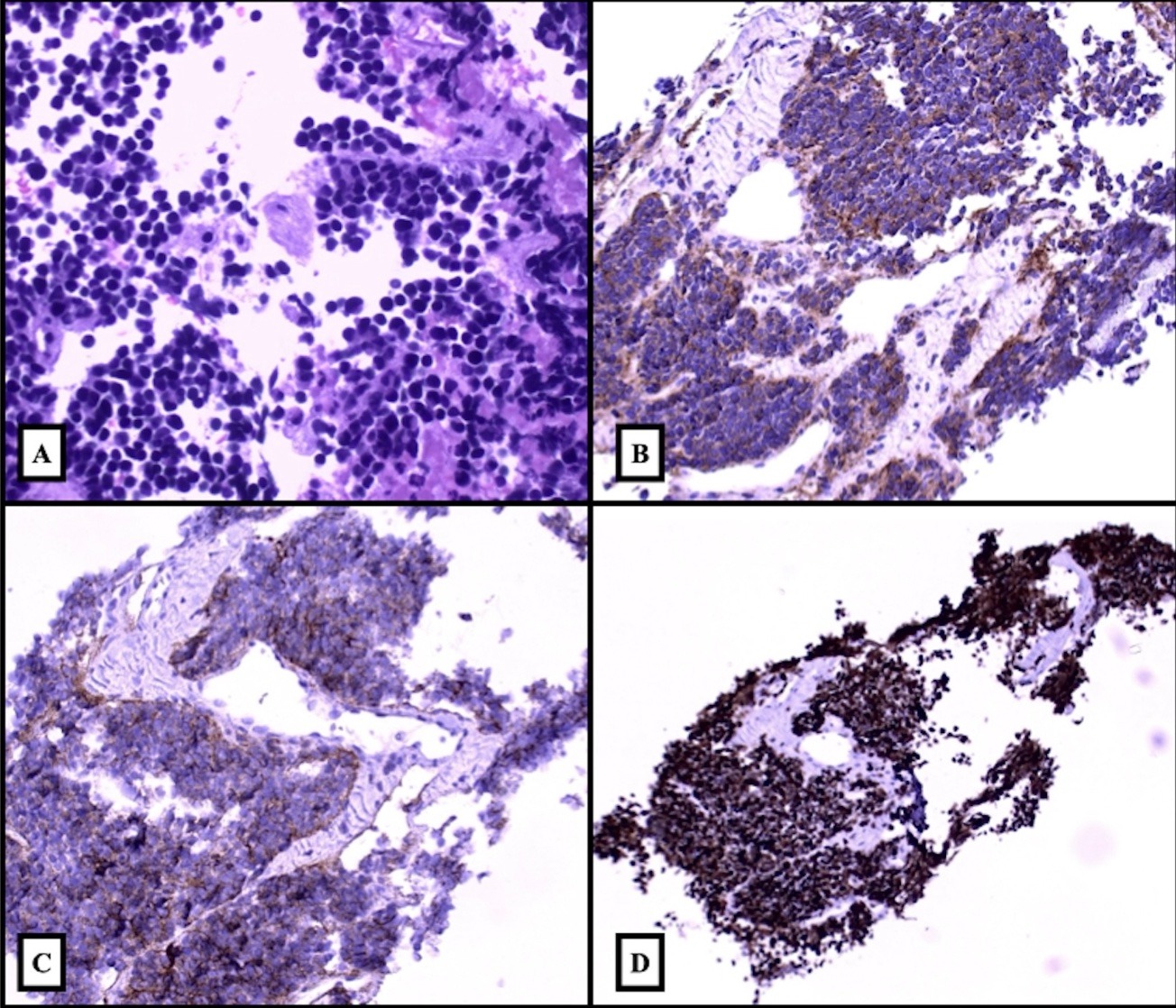
Case Description/Methods: A 62-year-old female with a history of morbid obesity status-post gastric sleeve presented with diffuse abdominal pain, nausea, coffee-ground emesis, black stools for the past few days as well as 20-pound weight loss and decreased appetite over the past month. On arrival, she was hemodynamically stable. Physical exam was significant for right upper quadrant tenderness. Blood tests revealed a hemoglobin 10.1 g/dL, ALT/AST 244/406 U/L, ALP 759 U/L, BUN/Cr 46/2.1, total bilirubin 3.6 mg/dL. PT/INR 15/1.2. Hepatitis panel was negative. AFP and CEA were normal. CA 19-9 was 150 U/mL. CT abdomen/pelvis with contrast showed extensive liver lesions (largest 16 cm), with invasion of the gallbladder and pancreatic head resulting in common bile and pancreatic duct dilatation. ERCP for biliary stenting was done with normalization of AST, ALT and bilirubin. CT chest showed no lung pathology. EGD revealed minimal red blood at the GE junction likely due to Mallory-Weiss tear. IR-guided liver biopsy revealed SCC with tumor cells positive for CD56, synaptophysin but negative for chromogranin (Figure 1). Patient received 4 cycles of Cisplatin/Etoposide. Repeat CT showed decreased liver and gallbladder disease but new soft tissue in thoracic paravertebral/lower para-aortic area. She eventually expired 7 months after her diagnosis.
Discussion: SCC typically arises in the lungs and accounts for 25% of lung cancers. It is crucial to exclude lung SCC before diagnosing EPSCC, which represents 0.1-0.4% of all cancers. Diagnosing primary hepatic SCC, as in our patient, requires tissue biopsy with immunohistochemistry usually staining positive for neuroendocrine markers chromogranin, synaptophysin, and CD56. Treatment options for EPSCC remain elusive, although Carboplatin/Etoposide/Atezolizumab used in lung SCC may offer a potential therapeutic avenue. This case underscores the diagnostic challenges and therapeutic dilemmas encountered in managing this rare entity, necessitating further research to delineate optimal management strategies.
Disclosures:
Aboud Kaliounji, MD, Carla Hachicho, BA, Helena Saba, MD, Jude Noel, MD, Jenna Zudell, MD, Raavi Gupta, MD, Sushil Ahlawat, MD, MS, MBBS. P4802 - A Case of Primary Hepatic Small Cell Carcinoma Without Any Pulmonary Involvement: A Diagnostic Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Extrapulmonary small cell carcinoma (EPSCC) are extremely rare and account for 2-4% of all small cell carcinoma (SCC) cases, and even rarer in the liver and biliary tract which have been previously described only in a few case reports over the past few decades. The clinical, pathological and immunohisotchemical properties of liver SCC are not fully established. We present a case of a female with primary liver SCC presenting with abdominal pain and vomiting.
Case Description/Methods: A 62-year-old female with a history of morbid obesity status-post gastric sleeve presented with diffuse abdominal pain, nausea, coffee-ground emesis, black stools for the past few days as well as 20-pound weight loss and decreased appetite over the past month. On arrival, she was hemodynamically stable. Physical exam was significant for right upper quadrant tenderness. Blood tests revealed a hemoglobin 10.1 g/dL, ALT/AST 244/406 U/L, ALP 759 U/L, BUN/Cr 46/2.1, total bilirubin 3.6 mg/dL. PT/INR 15/1.2. Hepatitis panel was negative. AFP and CEA were normal. CA 19-9 was 150 U/mL. CT abdomen/pelvis with contrast showed extensive liver lesions (largest 16 cm), with invasion of the gallbladder and pancreatic head resulting in common bile and pancreatic duct dilatation. ERCP for biliary stenting was done with normalization of AST, ALT and bilirubin. CT chest showed no lung pathology. EGD revealed minimal red blood at the GE junction likely due to Mallory-Weiss tear. IR-guided liver biopsy revealed SCC with tumor cells positive for CD56, synaptophysin but negative for chromogranin (Figure 1). Patient received 4 cycles of Cisplatin/Etoposide. Repeat CT showed decreased liver and gallbladder disease but new soft tissue in thoracic paravertebral/lower para-aortic area. She eventually expired 7 months after her diagnosis.
Discussion: SCC typically arises in the lungs and accounts for 25% of lung cancers. It is crucial to exclude lung SCC before diagnosing EPSCC, which represents 0.1-0.4% of all cancers. Diagnosing primary hepatic SCC, as in our patient, requires tissue biopsy with immunohistochemistry usually staining positive for neuroendocrine markers chromogranin, synaptophysin, and CD56. Treatment options for EPSCC remain elusive, although Carboplatin/Etoposide/Atezolizumab used in lung SCC may offer a potential therapeutic avenue. This case underscores the diagnostic challenges and therapeutic dilemmas encountered in managing this rare entity, necessitating further research to delineate optimal management strategies.
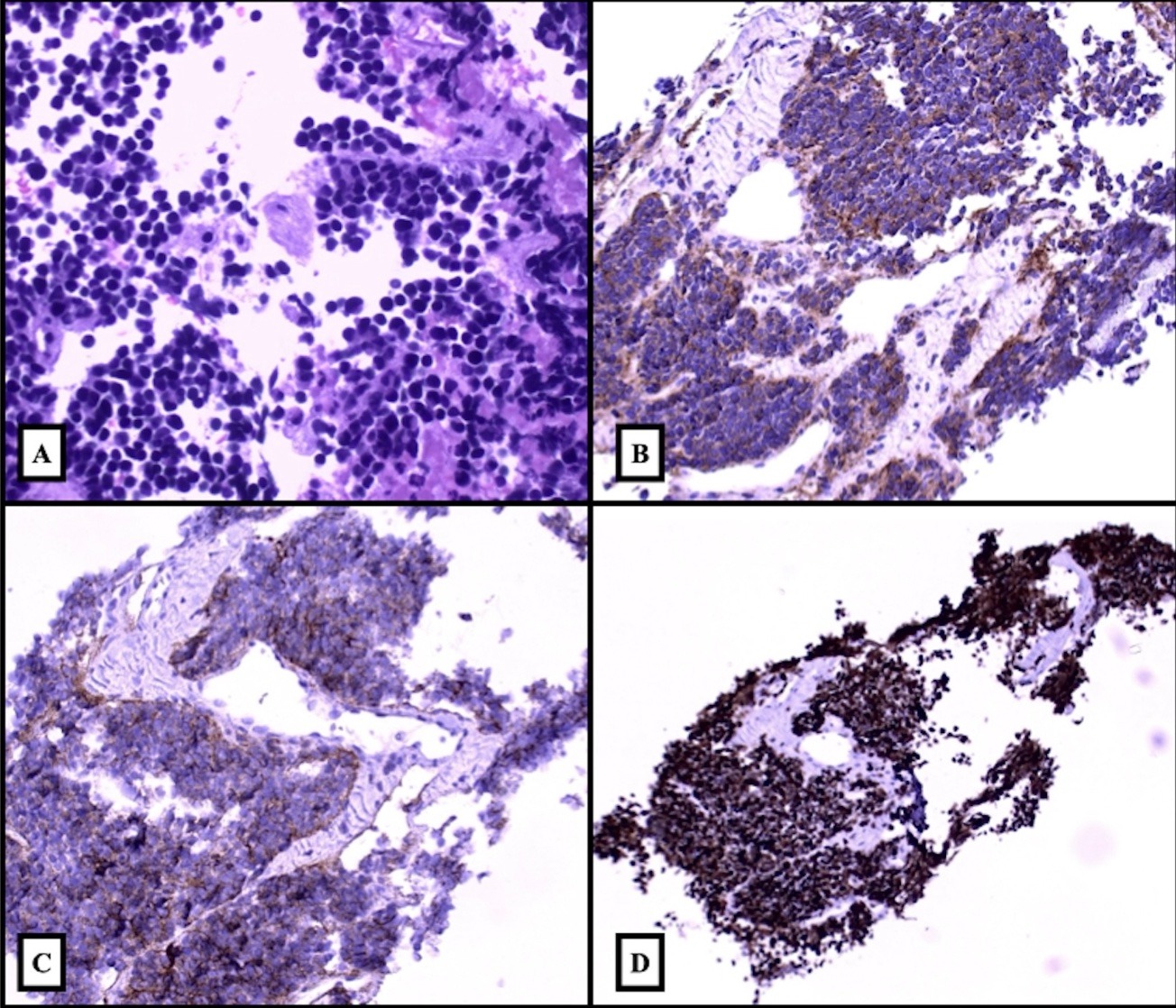
Figure: Figure 1: Histopathologic examination of hepatic mass.
1A. Sheets of small round tumor cells with scant cytoplasm (H&E 40x).
1B. Synaptophysin immunostain shows positive cytoplasmic staining (20x).
1C. CD56 immunostain shows positive membranous staining (20x).
1D. Ki67 exhibits a high proliferation index (99%) (10x).
1A. Sheets of small round tumor cells with scant cytoplasm (H&E 40x).
1B. Synaptophysin immunostain shows positive cytoplasmic staining (20x).
1C. CD56 immunostain shows positive membranous staining (20x).
1D. Ki67 exhibits a high proliferation index (99%) (10x).
Disclosures:
Aboud Kaliounji indicated no relevant financial relationships.
Carla Hachicho indicated no relevant financial relationships.
Helena Saba indicated no relevant financial relationships.
Jude Noel indicated no relevant financial relationships.
Jenna Zudell indicated no relevant financial relationships.
Raavi Gupta indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Aboud Kaliounji, MD, Carla Hachicho, BA, Helena Saba, MD, Jude Noel, MD, Jenna Zudell, MD, Raavi Gupta, MD, Sushil Ahlawat, MD, MS, MBBS. P4802 - A Case of Primary Hepatic Small Cell Carcinoma Without Any Pulmonary Involvement: A Diagnostic Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
