Tuesday Poster Session
Category: Liver
P4808 - A Case of Non-Cirrhotic Portal Hypertension in the Setting of Cavernous Transformation of Portal Vein Secondary to Portal Vein Thrombosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Amit Rajkarnikar, MD
Ochsner LSU Health
Lafayette, LA
Presenting Author(s)
Amit Rajkarnikar, MD1, Ahmad Anbar, MD1, Nadjel Opamen, MD1, Melanie Bienvenu, MD, MPH2
1Ochsner LSU Health, Lafayette, LA; 2LSU Health New Orleans School of Medicine, Lafayette, LA
Introduction: Cavernous Transformation of the Portal Vein (CTPV) is a rare condition with various etiologies. It occurs with long-standing portal vein thrombosis (PVT) which causes portal hypertension and an occlusion of the portal vein leading to the development and dilatation of multiple small vessels in and around the re-canalizing main portal vein. In this case, patient presented with abnormal uterine bleeding and symptomatic anemia with a history of prolonged anticoagulation for history of portal vein thrombosis with insidious cavernous transformation. The purpose of the case is to elucidate the dilemma about anticoagulation in patients with complication such as esophageal varices and AUB and approach therapy on a case-by-case basis.
Case Description/Methods: A 45-year-old female with PMH of portal vein thrombosis, esophageal varices, bipolar disorder, and anxiety was sent from GYN clinic to the ED after she was informed of her low hemoglobin and hematocrit. She had increased uterine bleeding that started few weeks before presentation and had been persistent. She had been changing her pad at least once approximately every 3 hours and noted blood clots intermittently. There were no alleviating or aggravating factors for her bleeding. There was no associated abdominal or vaginal pain. No hematemesis, melena or hematochezia were endorsed.Her H&H was Hemoglobin 4.4, Hematocrit 16. She received 3 units pRBC that corrected her symptomatic anemia. She was diagnosed with PVT in 2017 for which she was started on Warfarin. 2018 She had her hyper-coagulability workup that was essentially negative. She was switched to Xarelto daily thereafter. For her AUB gynecology workup was done with limited findings. US pelvis revealed 2 fibroids but TVUS not yet performed. Endometrial biopsy revealed benign findings. She has been started on Provera 10 mg daily and Depo Provera shots.
Discussion: While patients with chronic PVT are often at risk for recurrent thrombosis, they are also at risk for bleeding. The decision to start and continue anticoagulation should be made case-by-case basis. The aim of anticoagulation in is to prevent recurrent thrombosis or extension to other splanchnic veins thereby preventing portal hypertension-related complications. The decision was made in our case to continue with anticoagulation for the fact that etiology of her portal vein thrombosis has yet to be determined. Further workup such as Fibroscan and liver biopsy and repeat hypercoagulability workup were discussed with patient going forward.
Disclosures:
Amit Rajkarnikar, MD1, Ahmad Anbar, MD1, Nadjel Opamen, MD1, Melanie Bienvenu, MD, MPH2. P4808 - A Case of Non-Cirrhotic Portal Hypertension in the Setting of Cavernous Transformation of Portal Vein Secondary to Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ochsner LSU Health, Lafayette, LA; 2LSU Health New Orleans School of Medicine, Lafayette, LA
Introduction: Cavernous Transformation of the Portal Vein (CTPV) is a rare condition with various etiologies. It occurs with long-standing portal vein thrombosis (PVT) which causes portal hypertension and an occlusion of the portal vein leading to the development and dilatation of multiple small vessels in and around the re-canalizing main portal vein. In this case, patient presented with abnormal uterine bleeding and symptomatic anemia with a history of prolonged anticoagulation for history of portal vein thrombosis with insidious cavernous transformation. The purpose of the case is to elucidate the dilemma about anticoagulation in patients with complication such as esophageal varices and AUB and approach therapy on a case-by-case basis.
Case Description/Methods: A 45-year-old female with PMH of portal vein thrombosis, esophageal varices, bipolar disorder, and anxiety was sent from GYN clinic to the ED after she was informed of her low hemoglobin and hematocrit. She had increased uterine bleeding that started few weeks before presentation and had been persistent. She had been changing her pad at least once approximately every 3 hours and noted blood clots intermittently. There were no alleviating or aggravating factors for her bleeding. There was no associated abdominal or vaginal pain. No hematemesis, melena or hematochezia were endorsed.Her H&H was Hemoglobin 4.4, Hematocrit 16. She received 3 units pRBC that corrected her symptomatic anemia. She was diagnosed with PVT in 2017 for which she was started on Warfarin. 2018 She had her hyper-coagulability workup that was essentially negative. She was switched to Xarelto daily thereafter. For her AUB gynecology workup was done with limited findings. US pelvis revealed 2 fibroids but TVUS not yet performed. Endometrial biopsy revealed benign findings. She has been started on Provera 10 mg daily and Depo Provera shots.
Discussion: While patients with chronic PVT are often at risk for recurrent thrombosis, they are also at risk for bleeding. The decision to start and continue anticoagulation should be made case-by-case basis. The aim of anticoagulation in is to prevent recurrent thrombosis or extension to other splanchnic veins thereby preventing portal hypertension-related complications. The decision was made in our case to continue with anticoagulation for the fact that etiology of her portal vein thrombosis has yet to be determined. Further workup such as Fibroscan and liver biopsy and repeat hypercoagulability workup were discussed with patient going forward.
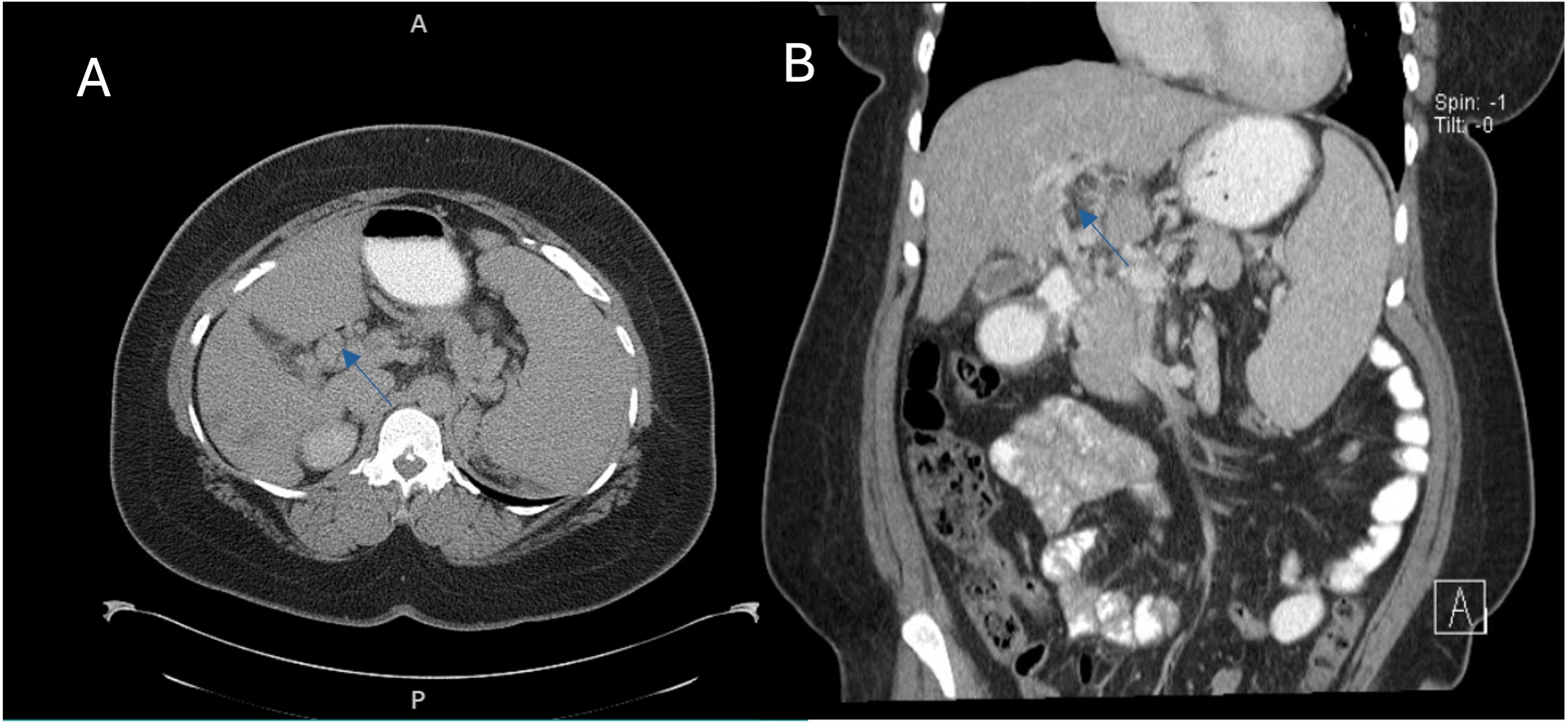
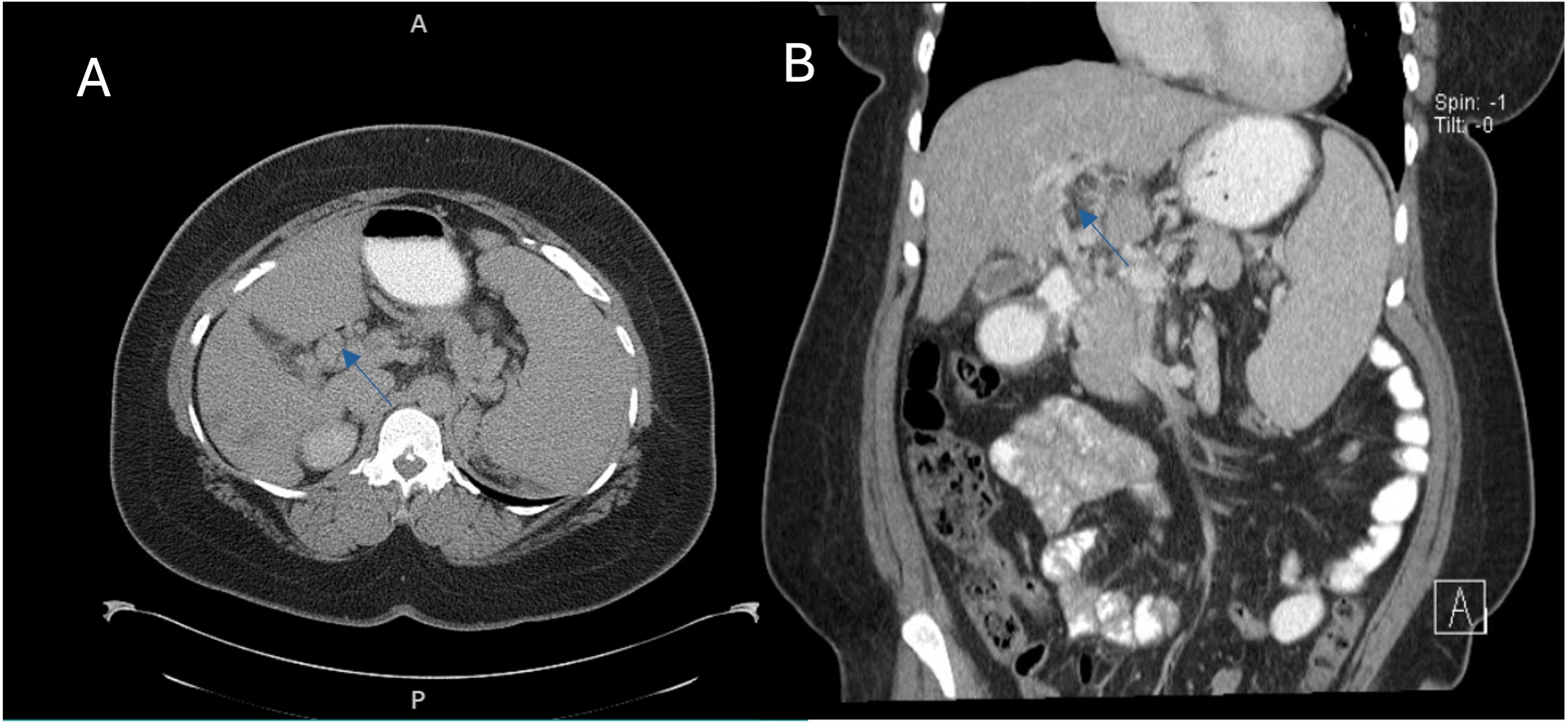
Figure: Fig A and B: Cavernous transformation of the portal vein is present. Numerous dilated varices throughout the periportal region, splenic hilum, and gastroesophageal region, splenomegaly, and cholelithiasis present.
Disclosures:
Amit Rajkarnikar indicated no relevant financial relationships.
Ahmad Anbar indicated no relevant financial relationships.
Nadjel Opamen indicated no relevant financial relationships.
Melanie Bienvenu indicated no relevant financial relationships.
Amit Rajkarnikar, MD1, Ahmad Anbar, MD1, Nadjel Opamen, MD1, Melanie Bienvenu, MD, MPH2. P4808 - A Case of Non-Cirrhotic Portal Hypertension in the Setting of Cavernous Transformation of Portal Vein Secondary to Portal Vein Thrombosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
