Tuesday Poster Session
Category: Liver
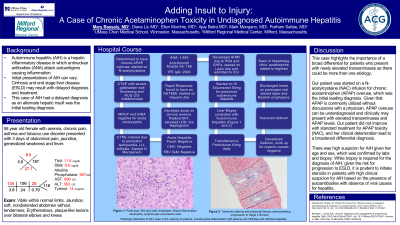
P4831 - Adding Insult to Injury: A Case of Chronic Acetaminophen Toxicity in Undiagnosed Autoimmune Hepatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mary Bassaly, MD
University of Massachusetts Chan Medical School, MA
Presenting Author(s)
Mary Bassaly, MD1, Mark M. Mangano, MD2, Ellen Murchie, MD1, Diana Liu, MD1, Ajay Batra, MD3, Parham Safaie, MD4
1University of Massachusetts Chan Medical School, Worcester, MA; 2Brigham and Women's Hospital, Wayland, MA; 3Milford Gastroenterology Assosciates, Hopkinton, MA; 4Milford Gastroenterology Associates, Milford, MA
Introduction: Autoimmune hepatitis (AIH) is a hepatic inflammatory disease in which antinuclear antibodies (ANA) attack autoantigens causing inflammation. Cirrhosis and end stage liver disease (ESLD) may result with delayed diagnosis and treatment. This case of AIH had a delayed diagnosis as an alternate hepatic insult was the initial leading diagnosis.
Case Description/Methods: A 58-year-old female with anemia and chronic pain presented with 3 days of abdominal pain, generalized weakness, and jaundice. She denied alcohol use. Initial labs showed elevated aspartate aminotransferase (896 U/L), alanine transaminase (562 U/L), alkaline phosphatase (987 U/L), acetaminophen (APAP) level (14 mcg/mL), direct (8.6 mg/dL) and total (11.8 mg/dL) bilirubin. Abdominal imaging showed gallbladder wall thickening; a hepatobiliary iminodiacetic acid scan (HIDA) was negative for acute cholecystitis. Acute hepatitis panel and other infectious hepatitis labs were negative. She was started on a N-acetylcysteine (NAC) infusion for chronic APAP overuse.Further workup showed ANA titer of 1:640, anti-smooth muscle antibody (ASMA) level of 156, and immunofixation immunoglobulin G (IFE IgG) of 2993 mg/dL. Intravenous (IV) steroids were started. Medical instability from non-ST elevation myocardial infarction, acute on chronic anemia and acute hypoxic respiratory failure, delayed liver biopsy.
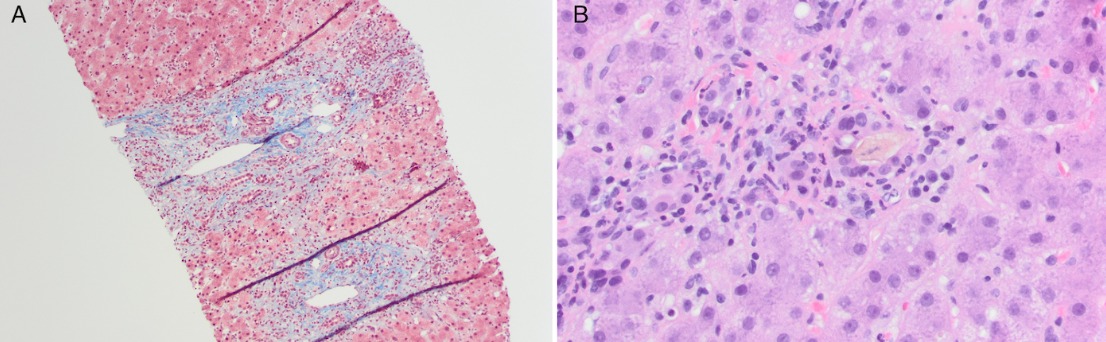
Subsequent liver biopsy was consistent with AIH (Figure 1A and 1B). She was eventually discharged on a prolonged oral steroid taper along with antibiotic prophylaxis and recently started azathioprine out patient.
Discussion: This case highlights the importance of a broad differential for patients who present with newly elevated transaminases as there could be more than one etiology.
Repeated supratherapeutic dosing of APAP can be underdiagnosed given that APAP is often utilized without discussions with a physician. As with our patient, chronic APAP overuse may present with elevated transaminases and APAP levels. Our patient did not improve with standard treatment for APAP toxicity (NAC), leading to a broadened differential diagnosis.
There was high suspicion for AIH given her age and sex, which was confirmed by labs and biopsy. While biopsy is required for the diagnosis of AIH, given the risk for progression to ESLD, it is prudent to initiate steroids in patients with high clinical suspicion for AIH based on the presence of autoantibodies and IgG with absence of viral causes for hepatitis.
Disclosures:
Mary Bassaly, MD1, Mark M. Mangano, MD2, Ellen Murchie, MD1, Diana Liu, MD1, Ajay Batra, MD3, Parham Safaie, MD4. P4831 - Adding Insult to Injury: A Case of Chronic Acetaminophen Toxicity in Undiagnosed Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School, Worcester, MA; 2Brigham and Women's Hospital, Wayland, MA; 3Milford Gastroenterology Assosciates, Hopkinton, MA; 4Milford Gastroenterology Associates, Milford, MA
Introduction: Autoimmune hepatitis (AIH) is a hepatic inflammatory disease in which antinuclear antibodies (ANA) attack autoantigens causing inflammation. Cirrhosis and end stage liver disease (ESLD) may result with delayed diagnosis and treatment. This case of AIH had a delayed diagnosis as an alternate hepatic insult was the initial leading diagnosis.
Case Description/Methods: A 58-year-old female with anemia and chronic pain presented with 3 days of abdominal pain, generalized weakness, and jaundice. She denied alcohol use. Initial labs showed elevated aspartate aminotransferase (896 U/L), alanine transaminase (562 U/L), alkaline phosphatase (987 U/L), acetaminophen (APAP) level (14 mcg/mL), direct (8.6 mg/dL) and total (11.8 mg/dL) bilirubin. Abdominal imaging showed gallbladder wall thickening; a hepatobiliary iminodiacetic acid scan (HIDA) was negative for acute cholecystitis. Acute hepatitis panel and other infectious hepatitis labs were negative. She was started on a N-acetylcysteine (NAC) infusion for chronic APAP overuse.Further workup showed ANA titer of 1:640, anti-smooth muscle antibody (ASMA) level of 156, and immunofixation immunoglobulin G (IFE IgG) of 2993 mg/dL. Intravenous (IV) steroids were started. Medical instability from non-ST elevation myocardial infarction, acute on chronic anemia and acute hypoxic respiratory failure, delayed liver biopsy.
Subsequent liver biopsy was consistent with AIH (Figure 1A and 1B). She was eventually discharged on a prolonged oral steroid taper along with antibiotic prophylaxis and recently started azathioprine out patient.
Discussion: This case highlights the importance of a broad differential for patients who present with newly elevated transaminases as there could be more than one etiology.
Repeated supratherapeutic dosing of APAP can be underdiagnosed given that APAP is often utilized without discussions with a physician. As with our patient, chronic APAP overuse may present with elevated transaminases and APAP levels. Our patient did not improve with standard treatment for APAP toxicity (NAC), leading to a broadened differential diagnosis.
There was high suspicion for AIH given her age and sex, which was confirmed by labs and biopsy. While biopsy is required for the diagnosis of AIH, given the risk for progression to ESLD, it is prudent to initiate steroids in patients with high clinical suspicion for AIH based on the presence of autoantibodies and IgG with absence of viral causes for hepatitis.
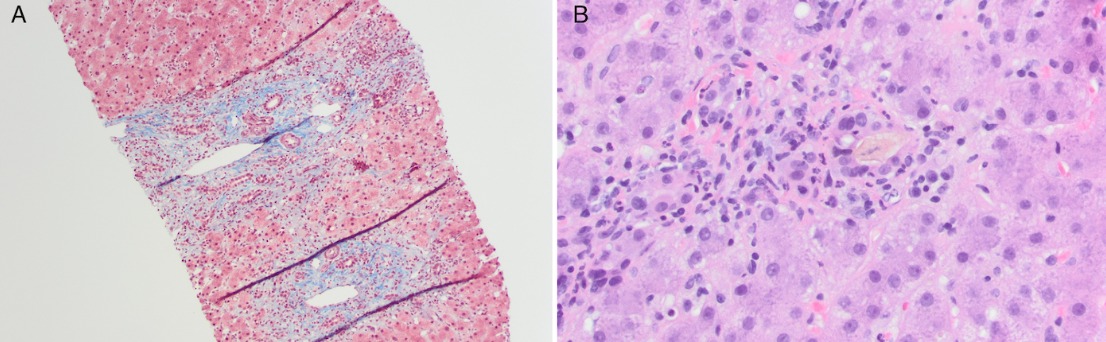
Figure: Figure 1:
A: Trichrome staining with periportal fibrosis (demonstrating progression to Stage 2 fibrosis).
B: Portal area. Bile duct with cholestasis. Mixed inflammation neutrophils, lymphocytes and plasma cells.
A: Trichrome staining with periportal fibrosis (demonstrating progression to Stage 2 fibrosis).
B: Portal area. Bile duct with cholestasis. Mixed inflammation neutrophils, lymphocytes and plasma cells.
Disclosures:
Mary Bassaly indicated no relevant financial relationships.
Mark Mangano indicated no relevant financial relationships.
Ellen Murchie indicated no relevant financial relationships.
Diana Liu indicated no relevant financial relationships.
Ajay Batra indicated no relevant financial relationships.
Parham Safaie indicated no relevant financial relationships.
Mary Bassaly, MD1, Mark M. Mangano, MD2, Ellen Murchie, MD1, Diana Liu, MD1, Ajay Batra, MD3, Parham Safaie, MD4. P4831 - Adding Insult to Injury: A Case of Chronic Acetaminophen Toxicity in Undiagnosed Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
