Tuesday Poster Session
Category: Liver
P4841 - Semaglutide Shadows: A Rare Glimpse Into GLP-1-Associated Liver Injury
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harsimran Kalsi, MBBS
University of Central Florida College of Medicine
Gainesville, FL
Presenting Author(s)
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Raghav Bassi, MD1, Mohammad Abuassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1
1University of Central Florida College of Medicine, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL
Introduction: Drug-induced liver injury (DILI) is a rare but serious complication that poses diagnostic challenges due to its varied presentation and broad differential diagnosis. DILI can result from direct intrinsic hepatotoxicity or idiosyncratic reactions, making it a challenging disease to diagnose and a leading cause of acute liver failure. Semaglutide has been approved by the United States Food and Drug Administration for managing obesity and type -2 diabetes mellitus. Semaglutide is generally well-tolerated but can lead to gastrointestinal distress, dyspepsia, pancreatitis, gastroparesis. Although uncommon, GLP-1 agonists have been associated with hepatotoxicity. We describe a rare case of semaglutide-induced liver injury, elucidating the diagnostic conundrum and therapeutic approach.
Case Description/Methods: A 44-year-old female with no significant medical history presented with jaundice, fatigue, and itching, alongside elevated liver enzymes—recurring symptoms from six months prior when she had similar laboratory anomalies. Initial workup was negative for viral hepatitis and autoimmune markers except a high ferritin level (1783 ng/ml). Her liver enzymes and symptoms improved on discontinuing semaglutide, which she was taking for weight loss.
During her current hospitalization, despite abstaining from tobacco, alcohol, she had markedly elevated AST (760 IU/L), ALT (1459 IU/L), and bilirubin levels (Total 11.1 mg/dl, Direct 8.3 mg/dl). Viral hepatitis panel and autoimmune workup was negative. CTAP and MRCP ruled out other hepatic pathologies. Liver biopsy findings indicated acute hepatitis with mononuclear infiltrate and necrosis, pointing to drug-induced liver injury. Treatment with fluids led to improved liver enzymes at discharge. Four weeks follow-up showed normalization of liver tests, confirming the reversible nature of semaglutide-induced liver injury with timely management.
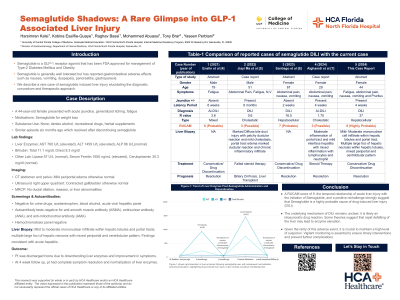
Discussion: Semaglutide-induced liver injury is a rare entity that requires a high index of suspicion and a methodical approach to diagnosis. On literature review, there were four other reported cases of semaglutide induced DILI. (Table-1).
Given the rarity of this adverse event, maintaining a high level of suspicion is crucial, particularly when there is a temporal association between the onset of symptoms and the initiation of a GLP-1a treatment, and after other more common etiologies have been excluded. This vigilance is essential to ensure timely intervention and prevent further complications.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Raghav Bassi, MD1, Mohammad Abuassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1. P4841 - Semaglutide Shadows: A Rare Glimpse Into GLP-1-Associated Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Central Florida College of Medicine, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL
Introduction: Drug-induced liver injury (DILI) is a rare but serious complication that poses diagnostic challenges due to its varied presentation and broad differential diagnosis. DILI can result from direct intrinsic hepatotoxicity or idiosyncratic reactions, making it a challenging disease to diagnose and a leading cause of acute liver failure. Semaglutide has been approved by the United States Food and Drug Administration for managing obesity and type -2 diabetes mellitus. Semaglutide is generally well-tolerated but can lead to gastrointestinal distress, dyspepsia, pancreatitis, gastroparesis. Although uncommon, GLP-1 agonists have been associated with hepatotoxicity. We describe a rare case of semaglutide-induced liver injury, elucidating the diagnostic conundrum and therapeutic approach.
Case Description/Methods: A 44-year-old female with no significant medical history presented with jaundice, fatigue, and itching, alongside elevated liver enzymes—recurring symptoms from six months prior when she had similar laboratory anomalies. Initial workup was negative for viral hepatitis and autoimmune markers except a high ferritin level (1783 ng/ml). Her liver enzymes and symptoms improved on discontinuing semaglutide, which she was taking for weight loss.
During her current hospitalization, despite abstaining from tobacco, alcohol, she had markedly elevated AST (760 IU/L), ALT (1459 IU/L), and bilirubin levels (Total 11.1 mg/dl, Direct 8.3 mg/dl). Viral hepatitis panel and autoimmune workup was negative. CTAP and MRCP ruled out other hepatic pathologies. Liver biopsy findings indicated acute hepatitis with mononuclear infiltrate and necrosis, pointing to drug-induced liver injury. Treatment with fluids led to improved liver enzymes at discharge. Four weeks follow-up showed normalization of liver tests, confirming the reversible nature of semaglutide-induced liver injury with timely management.
Discussion: Semaglutide-induced liver injury is a rare entity that requires a high index of suspicion and a methodical approach to diagnosis. On literature review, there were four other reported cases of semaglutide induced DILI. (Table-1).
Given the rarity of this adverse event, maintaining a high level of suspicion is crucial, particularly when there is a temporal association between the onset of symptoms and the initiation of a GLP-1a treatment, and after other more common etiologies have been excluded. This vigilance is essential to ensure timely intervention and prevent further complications.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Raghav Bassi indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Harsimran Kalsi, MBBS1, Kobina Essilfie-Quaye, MD1, Raghav Bassi, MD1, Mohammad Abuassi, MD1, Yaseen Perbtani, DO2, Tony S.. Brar, MD1. P4841 - Semaglutide Shadows: A Rare Glimpse Into GLP-1-Associated Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
