Tuesday Poster Session
Category: Liver
P4850 - Navigating Complexity: Overlap of Autoimmune Hepatitis and Systemic Lupus Erythematosus
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Ali Butt, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Muhammad Ali Butt, MD1, Chandan K. Dash, MD1, Taimur Muzammil, MD1, Nabeeha Mohy-ud-din, MD2
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
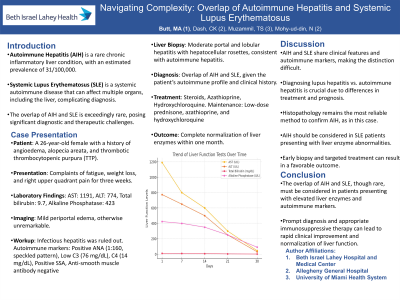
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory disease of the liver with low prevalence (31/100,000 cases). Systemic Lupus Erythematosus (SLE) is a systemic disease that involves multiple organs, and patients can have elevated LFTs from multiple causes including ‘lupus hepatitis’. The overlap between AIH and SLE is even rarer, and can prove to be a diagnostic and therapeutic challenge.
Case Description/Methods: A 26-year-old female with a past medical history of angioedema, alopecia areata, and Thrombotic Thrombocytopenic Purpura (TTP) presented to the hospital with complaints of fatigue, weight loss, and three weeks of right upper quadrant discomfort. Initial laboratory workup revealed markedly elevated liver enzymes (AST 1191, ALT 774), high total bilirubin (9.7), and elevated Alkaline Phosphatase levels (423). Her imaging was unremarkable except mild periportal edema. Extensive workup for infectious hepatitis was negative. Autoimmune workup revealed positive ANA (1:160, speckled pattern), low C3 (76 mg/dL), low C4 (14 mg/dL), Anti-smooth muscle antibody (< 1:20), IgG 782 and positive Sjogren’s Syndrome Antibody (SSA). Subsequent ultrasound-guided liver biopsy confirmed moderate portal and lobular hepatitis with hepatocellular rosettes and interface hepatitis consistent with autoimmune hepatitis. Given the patient's autoimmune profile (ANA, SSA positivity, and hypocomplementemia), alongside a history of angioedema and unprovoked TTP, a diagnosis of Systemic Lupus Erythematosus (SLE) with concomitant autoimmune hepatitis was established. The patient was initiated on steroids, and azathioprine and hydroxychloroquine were added to her treatment regimen. Her liver function tests normalized over a month, and she is currently maintained on low-dose prednisone, azathioprine, and hydroxychloroquine.
Discussion: AIH and SLE are distinct yet overlapping conditions, presenting challenges in diagnosis and management due to shared clinical features and diagnostic markers. Distinguishing between autoimmune hepatitis and lupus hepatitis is crucial, as their complications, prognosis, and treatment strategies vary. Histopathological examination of liver biopsy samples remains the most reliable method for differentiation. This case highlights the need for consideration of AIH in the differential diagnosis of SLE patients presenting with elevated liver enzymes.
Disclosures:
Muhammad Ali Butt, MD1, Chandan K. Dash, MD1, Taimur Muzammil, MD1, Nabeeha Mohy-ud-din, MD2. P4850 - Navigating Complexity: Overlap of Autoimmune Hepatitis and Systemic Lupus Erythematosus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory disease of the liver with low prevalence (31/100,000 cases). Systemic Lupus Erythematosus (SLE) is a systemic disease that involves multiple organs, and patients can have elevated LFTs from multiple causes including ‘lupus hepatitis’. The overlap between AIH and SLE is even rarer, and can prove to be a diagnostic and therapeutic challenge.
Case Description/Methods: A 26-year-old female with a past medical history of angioedema, alopecia areata, and Thrombotic Thrombocytopenic Purpura (TTP) presented to the hospital with complaints of fatigue, weight loss, and three weeks of right upper quadrant discomfort. Initial laboratory workup revealed markedly elevated liver enzymes (AST 1191, ALT 774), high total bilirubin (9.7), and elevated Alkaline Phosphatase levels (423). Her imaging was unremarkable except mild periportal edema. Extensive workup for infectious hepatitis was negative. Autoimmune workup revealed positive ANA (1:160, speckled pattern), low C3 (76 mg/dL), low C4 (14 mg/dL), Anti-smooth muscle antibody (< 1:20), IgG 782 and positive Sjogren’s Syndrome Antibody (SSA). Subsequent ultrasound-guided liver biopsy confirmed moderate portal and lobular hepatitis with hepatocellular rosettes and interface hepatitis consistent with autoimmune hepatitis. Given the patient's autoimmune profile (ANA, SSA positivity, and hypocomplementemia), alongside a history of angioedema and unprovoked TTP, a diagnosis of Systemic Lupus Erythematosus (SLE) with concomitant autoimmune hepatitis was established. The patient was initiated on steroids, and azathioprine and hydroxychloroquine were added to her treatment regimen. Her liver function tests normalized over a month, and she is currently maintained on low-dose prednisone, azathioprine, and hydroxychloroquine.
Discussion: AIH and SLE are distinct yet overlapping conditions, presenting challenges in diagnosis and management due to shared clinical features and diagnostic markers. Distinguishing between autoimmune hepatitis and lupus hepatitis is crucial, as their complications, prognosis, and treatment strategies vary. Histopathological examination of liver biopsy samples remains the most reliable method for differentiation. This case highlights the need for consideration of AIH in the differential diagnosis of SLE patients presenting with elevated liver enzymes.
Disclosures:
Muhammad Ali Butt indicated no relevant financial relationships.
Chandan Dash indicated no relevant financial relationships.
Taimur Muzammil indicated no relevant financial relationships.
Nabeeha Mohy-ud-din indicated no relevant financial relationships.
Muhammad Ali Butt, MD1, Chandan K. Dash, MD1, Taimur Muzammil, MD1, Nabeeha Mohy-ud-din, MD2. P4850 - Navigating Complexity: Overlap of Autoimmune Hepatitis and Systemic Lupus Erythematosus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
