Tuesday Poster Session
Category: Obesity
P4873 - Primary Care Physicians' Experiences of Obesity Counseling and Management in Culturally and Linguistically Diverse Populations
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HO
Haya Omeish, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Haya Omeish, MD1, Husam Bader, MD2, Rama Maghnam, MD2, Husam Barham, MD3, Joud Maghnam, MD4, Ahmad Al-Thunaibat, MD5, Ahmad Abu-Sulb, MD6
1Henry Ford Health, Detroit, MI; 2University of Michigan, Ann Arbor, MI; 3HCA Healthcare, Portsmouth, NH; 4Al-Balqa’ Applied University, Amman, 'Amman, Jordan; 5Hamilton Health Care System, Dalton, GA; 6Orlando Regional Medical Center, Orlando, FL
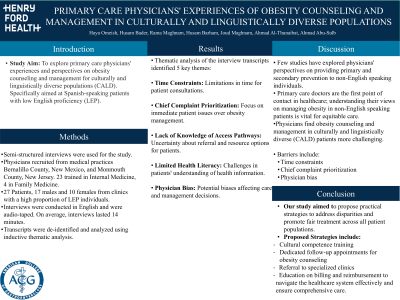
Introduction: The purpose of the study was to explore Primary care physicians’ experiences and perspectives of obesity counseling and management of culturally and linguistically diverse populations (CALD). Particularly in reference to Spanish speaking patients with low English proficiency (LEP).
Methods: Semi-structured interviews were employed to achieve the aim of this study. 27 interviews were conducted. Participants were recruited from medical practices in Bernalillo county, New Mexico and Monmouth county, New Jersey. All participants provided primary care in clinics with a large proportion of LEP individuals. Of the 27 physicians, 17 were males and 10 were females. 23 physicians were trained in Internal Medicine and 4 were trained in Family medicine. All providers were either American board certified or board eligible. All interviews were conducted in English while encounters were audio taped. All transcripts were de-identified, followed by inductive thematic analysis.
Results: On average, interviews lasted 14 minutes. Thematic analysis of the interview transcripts identified 5 key themes: time constraints, chief complaint prioritization, lack of knowledge of access pathways, limited health literacy, and physician bias.
Discussion: Few studies have investigated physicians' perspectives on delivering primary and secondary prevention to non-English speaking individuals. Primary care doctors are the first point of contact for healthcare, and understanding their views on managing obesity in non-English speaking patients is crucial for ensuring equitable care for minority groups.
Physicians perceive obesity counseling and management in culturally and linguistically diverse (CALD) patients to be more challenging. Identified barriers include time constraints, chief complaint prioritization, and physician bias.
This study aims to propose practical strategies to address this disparity and promote fair treatment across all patient populations. Strategies include cultural competence training, dedicated follow-up appointments to focus on obesity counseling, referral to specialized clinics, education on billing and reimbursement to help navigate the system more effectively and ensure comprehensive care.
Disclosures:
Haya Omeish, MD1, Husam Bader, MD2, Rama Maghnam, MD2, Husam Barham, MD3, Joud Maghnam, MD4, Ahmad Al-Thunaibat, MD5, Ahmad Abu-Sulb, MD6. P4873 - Primary Care Physicians' Experiences of Obesity Counseling and Management in Culturally and Linguistically Diverse Populations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2University of Michigan, Ann Arbor, MI; 3HCA Healthcare, Portsmouth, NH; 4Al-Balqa’ Applied University, Amman, 'Amman, Jordan; 5Hamilton Health Care System, Dalton, GA; 6Orlando Regional Medical Center, Orlando, FL
Introduction: The purpose of the study was to explore Primary care physicians’ experiences and perspectives of obesity counseling and management of culturally and linguistically diverse populations (CALD). Particularly in reference to Spanish speaking patients with low English proficiency (LEP).
Methods: Semi-structured interviews were employed to achieve the aim of this study. 27 interviews were conducted. Participants were recruited from medical practices in Bernalillo county, New Mexico and Monmouth county, New Jersey. All participants provided primary care in clinics with a large proportion of LEP individuals. Of the 27 physicians, 17 were males and 10 were females. 23 physicians were trained in Internal Medicine and 4 were trained in Family medicine. All providers were either American board certified or board eligible. All interviews were conducted in English while encounters were audio taped. All transcripts were de-identified, followed by inductive thematic analysis.
Results: On average, interviews lasted 14 minutes. Thematic analysis of the interview transcripts identified 5 key themes: time constraints, chief complaint prioritization, lack of knowledge of access pathways, limited health literacy, and physician bias.
Discussion: Few studies have investigated physicians' perspectives on delivering primary and secondary prevention to non-English speaking individuals. Primary care doctors are the first point of contact for healthcare, and understanding their views on managing obesity in non-English speaking patients is crucial for ensuring equitable care for minority groups.
Physicians perceive obesity counseling and management in culturally and linguistically diverse (CALD) patients to be more challenging. Identified barriers include time constraints, chief complaint prioritization, and physician bias.
This study aims to propose practical strategies to address this disparity and promote fair treatment across all patient populations. Strategies include cultural competence training, dedicated follow-up appointments to focus on obesity counseling, referral to specialized clinics, education on billing and reimbursement to help navigate the system more effectively and ensure comprehensive care.
Disclosures:
Haya Omeish indicated no relevant financial relationships.
Husam Bader indicated no relevant financial relationships.
Rama Maghnam indicated no relevant financial relationships.
Husam Barham indicated no relevant financial relationships.
Joud Maghnam indicated no relevant financial relationships.
Ahmad Al-Thunaibat indicated no relevant financial relationships.
Ahmad Abu-Sulb indicated no relevant financial relationships.
Haya Omeish, MD1, Husam Bader, MD2, Rama Maghnam, MD2, Husam Barham, MD3, Joud Maghnam, MD4, Ahmad Al-Thunaibat, MD5, Ahmad Abu-Sulb, MD6. P4873 - Primary Care Physicians' Experiences of Obesity Counseling and Management in Culturally and Linguistically Diverse Populations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
