Tuesday Poster Session
Category: Obesity
P4891 - Beyond Weight Loss: Exploring the Complications of Gastric Bypass Surgery - A Case of Gastrocolic Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E


Ibrar Atiq, MD
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
Ibrar Atiq, MD, Muhammad Ahmed, MD, Usama Sakhawat, MD, Yasir Ahmed, MD, Mohammad Abidi, MD, Leslie Bank, MD
United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Bariatric surgery for weight loss has become a common practice in the United States, with about 280,000 operations performed in 2022. To be a practicing health professional in the modern era, one must understand the more common chronic complications that may result from altering the gastrointestinal (GI) tract and how to manage these complications.
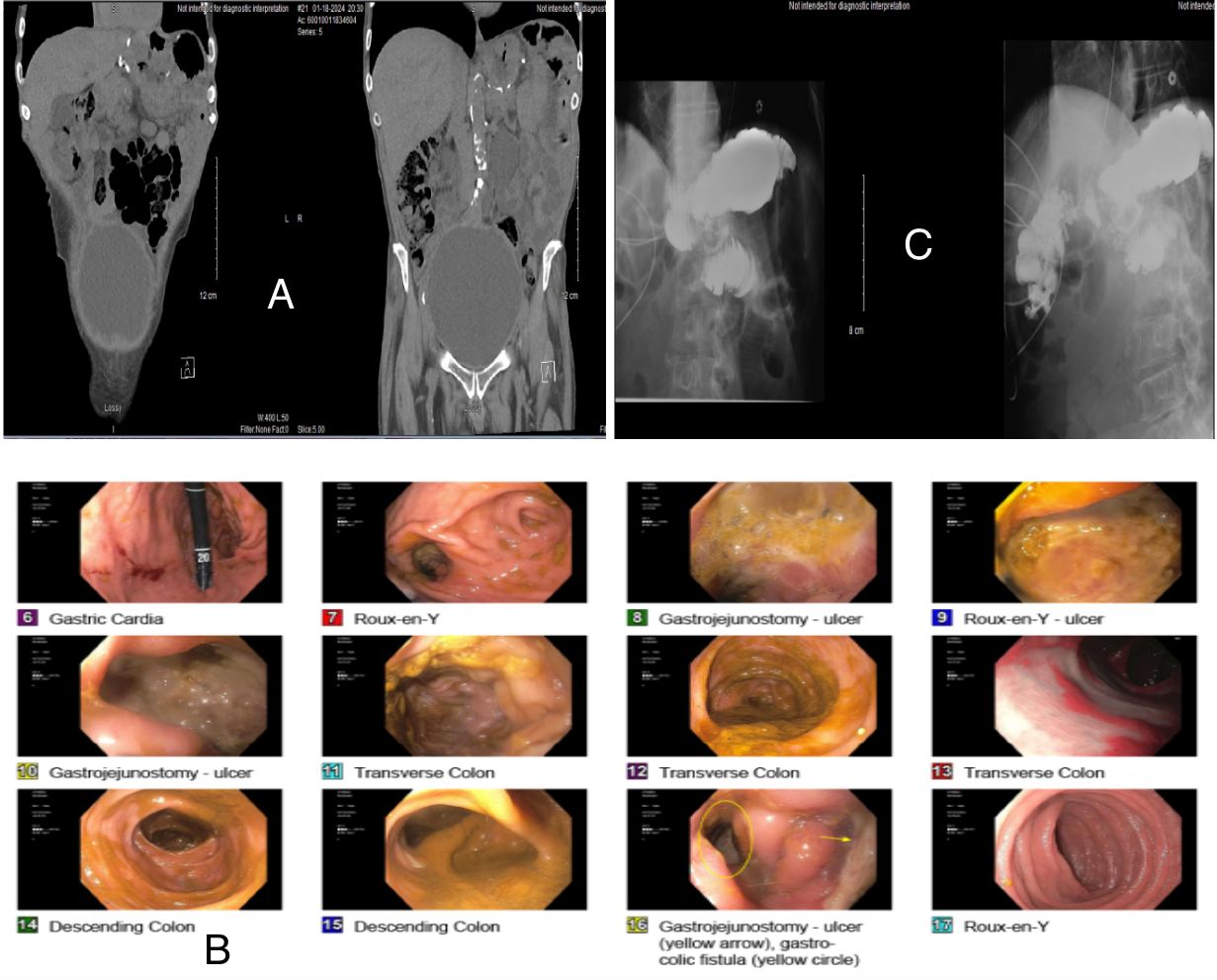
Case Description/Methods: A 63 year old male with medical history of Roux-en-Y gastric bypass (RYGB) in 1996 presented with a complaint of abdominal pain for 1 week and watery diarrhea 6-7 bowel movements/day for almost 1 year. He also admits weight loss of 30 pounds in 1 year but denies any hematochezia, melena, hematemesis, nausea, vomiting. On presentation, the patient was hemodynamically stable, Lab tests consistent with stable hemoglobin (Hb) 12.2 but elevated BUN/Cr 55/2.4. He had a CT abd/pelvis which was consistent with distended bladder and intrarenal ducts, also found to have diffuse enteritis [A]. Patient admitted for acute kidney injury, IV fluids were initiated and foley catheter was placed with improvement in his kidney functions but within the next couple of days patient’s Hb trended down, 12.2 to 8.4 without any overt signs of bleeding. Patient underwent Esophagogastroduodenoscopy (EGD) and Colonoscopy. On EGD, found to have Gastro jejunal anastomosis characterized by ulceration. A gastro-colic fistula (GCF) was noted at the gastro-jejunal anastomosis[B]. Colonoscopy findings were insignificant except noted to have GCF. Patient had an Upper GI series with small bowel FL which confirmed the evidence of GC fistula as there was eventual opacification of the colon in the right upper abdomen [C]. Patient underwent an Ex-lap with revision gastrojejunostomy. Postoperative course was uncomplicated and his symptoms improved.
Discussion: All gastric bypass surgeries have complications acute or chronic, for example Anastomotic Leak, Cholelithiasis, small bowel obstruction, Dumping syndrome, Marginal ulcers, Gastro-gastric or Gastrocolic fistula and nutritional deficiencies. GCF is a rare complication with an incidence of 0.6%. GCF is an abnormal connection of anastomotic site and colon. Pathophysiology is chronic fibrosis due to marginal ulcer, foreign body erosion and anastomotic leak. Typically presents with abdominal pain, diarrhea and weight loss. Diagnosis is confirmed with EGD and Upper GI study. Treatment includes Endoscopic intervention of small fistulae with clips may be successful; however, surgical treatment is usually necessary.
Disclosures:
Ibrar Atiq, MD, Muhammad Ahmed, MD, Usama Sakhawat, MD, Yasir Ahmed, MD, Mohammad Abidi, MD, Leslie Bank, MD. P4891 - Beyond Weight Loss: Exploring the Complications of Gastric Bypass Surgery - A Case of Gastrocolic Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Bariatric surgery for weight loss has become a common practice in the United States, with about 280,000 operations performed in 2022. To be a practicing health professional in the modern era, one must understand the more common chronic complications that may result from altering the gastrointestinal (GI) tract and how to manage these complications.
Case Description/Methods: A 63 year old male with medical history of Roux-en-Y gastric bypass (RYGB) in 1996 presented with a complaint of abdominal pain for 1 week and watery diarrhea 6-7 bowel movements/day for almost 1 year. He also admits weight loss of 30 pounds in 1 year but denies any hematochezia, melena, hematemesis, nausea, vomiting. On presentation, the patient was hemodynamically stable, Lab tests consistent with stable hemoglobin (Hb) 12.2 but elevated BUN/Cr 55/2.4. He had a CT abd/pelvis which was consistent with distended bladder and intrarenal ducts, also found to have diffuse enteritis [A]. Patient admitted for acute kidney injury, IV fluids were initiated and foley catheter was placed with improvement in his kidney functions but within the next couple of days patient’s Hb trended down, 12.2 to 8.4 without any overt signs of bleeding. Patient underwent Esophagogastroduodenoscopy (EGD) and Colonoscopy. On EGD, found to have Gastro jejunal anastomosis characterized by ulceration. A gastro-colic fistula (GCF) was noted at the gastro-jejunal anastomosis[B]. Colonoscopy findings were insignificant except noted to have GCF. Patient had an Upper GI series with small bowel FL which confirmed the evidence of GC fistula as there was eventual opacification of the colon in the right upper abdomen [C]. Patient underwent an Ex-lap with revision gastrojejunostomy. Postoperative course was uncomplicated and his symptoms improved.
Discussion: All gastric bypass surgeries have complications acute or chronic, for example Anastomotic Leak, Cholelithiasis, small bowel obstruction, Dumping syndrome, Marginal ulcers, Gastro-gastric or Gastrocolic fistula and nutritional deficiencies. GCF is a rare complication with an incidence of 0.6%. GCF is an abnormal connection of anastomotic site and colon. Pathophysiology is chronic fibrosis due to marginal ulcer, foreign body erosion and anastomotic leak. Typically presents with abdominal pain, diarrhea and weight loss. Diagnosis is confirmed with EGD and Upper GI study. Treatment includes Endoscopic intervention of small fistulae with clips may be successful; however, surgical treatment is usually necessary.
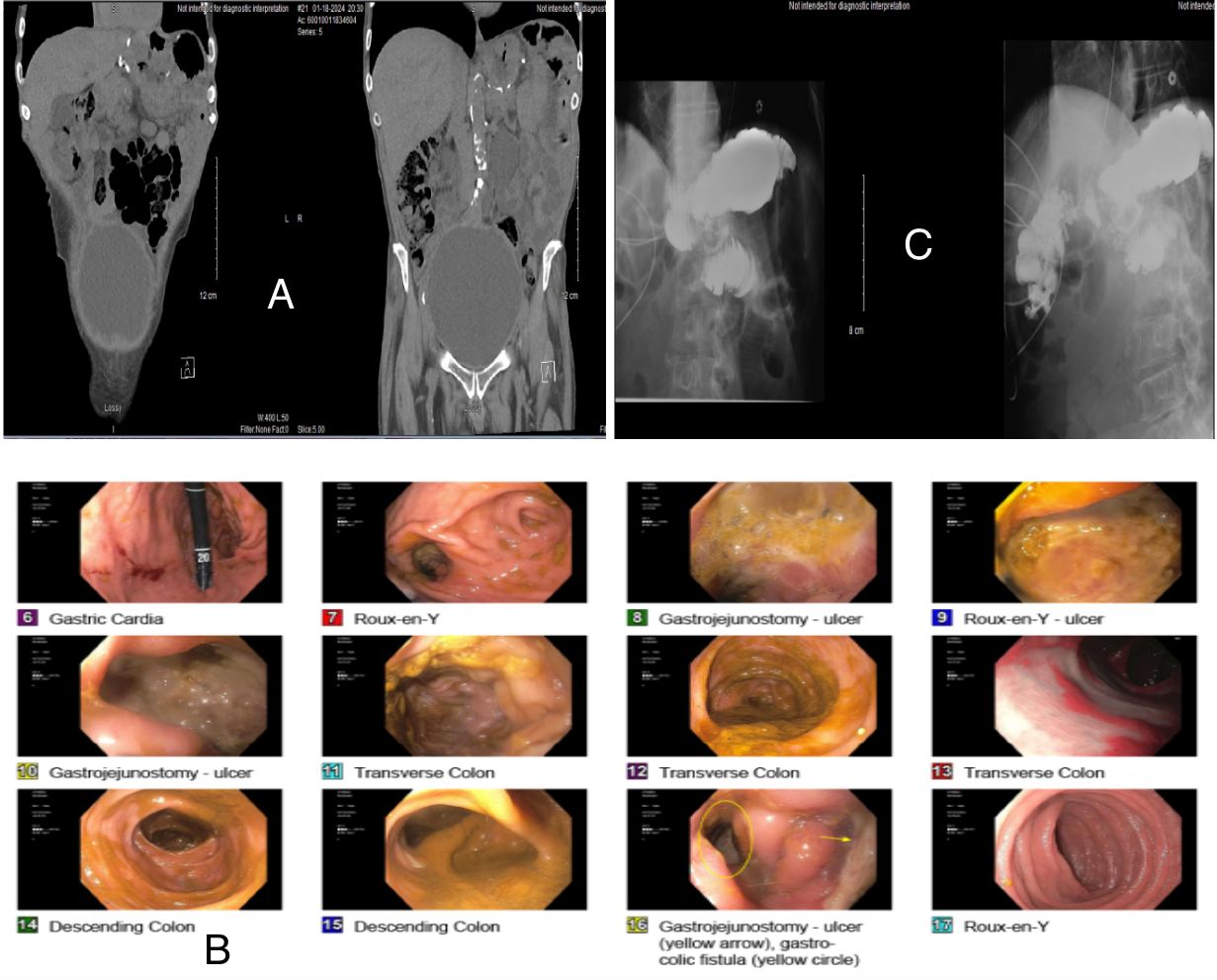
Figure: A. CAT abdomen pelvis with distended bladder and intra-renal ducts. Diffuse enteritis. B. Gastroscopy: Gastro jejunal anastomosis characterized by ulceration. A gastro-colic fistula (GCF) was noted at the gastro-jejunal anastomosis. C. Small bowel FL with evidence of GC fistula, eventual opacification of the colon in the right upper abdomen
Disclosures:
Ibrar Atiq indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Yasir Ahmed indicated no relevant financial relationships.
Mohammad Abidi indicated no relevant financial relationships.
Leslie Bank indicated no relevant financial relationships.
Ibrar Atiq, MD, Muhammad Ahmed, MD, Usama Sakhawat, MD, Yasir Ahmed, MD, Mohammad Abidi, MD, Leslie Bank, MD. P4891 - Beyond Weight Loss: Exploring the Complications of Gastric Bypass Surgery - A Case of Gastrocolic Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
